JAMA editorial and inaccurate media reports suggest
that cranberry has no value in preventing urinary tract infections
Reviewed: Juthani-Mehta M, Van Ness PH,
Bianco L, et al. Effect of cranberry capsules on bacteriuria plus pyuria among
older women in nursing homes: A randomized clinical trial. JAMA. 2016;316(18):1879-1887. doi:10.1001/jama.2016.16141.
On October 27, 2016, the Journal of the
American Medical Association (JAMA)
published online a randomized, double-blind, placebo-controlled clinical study
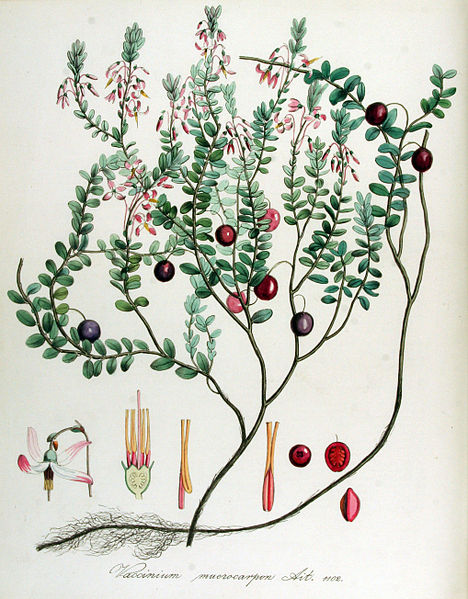
by Juthani-Mehta et al. from the Yale School of Medicine.1 The trial was designed to evaluate the effects of a cranberry (Vaccinium macrocarpon, Ericaceae) juice extract
preparation on bacteriuria plus pyuria (the presence of bacteria and pus in the
urine, respectively) in elderly female nursing home residents. The authors reported
that administration of two capsules of a standardized cranberry extract (Ellura
capsules, each containing 36 mg proanthocyanidins [PACs]; Pharmatoka; Rueil-Malmaison, France) for 12
months failed to provide a statistically significant difference in the
percentage of patients with bacteriuria and pyuria compared to placebo. The authors
also did not find any statistically significant differences in the secondary outcome
measures, such as symptomatic urinary tract infections (UTIs), mortality,
number of hospitalizations, presence of multi-drug resistant bacteria in the
urine, antibiotic treatments for suspected UTIs, and total antimicrobial
pharmaceutical drugs administered.

The study results have been covered, often uncritically, by major media outlets.
For example, an article in The New York
Times titled “The Cure for UTIs? It’s Not Cranberries” inaccurately generalized
the results of the study with its misleading headline.2 The study did not look at the effects of the cranberry extract
preparation to cure, or even treat, existing UTIs as the title of The New
York Times article suggests, but rather at its efficacy in the prevention
of bacteriuria and pyuria in older women.
According to data published by the same research group, 25-50% of women living
in nursing homes suffer from bacteriuria.3 Since clinical trials evaluating conventional antibiotic treatments
have not shown a reduction in urogenital infection-related diseases and deaths,
the current medical practice guidelines for institutionalized adults do not
recommend antibiotic treatments for bacteriuria or non-specific UTI symptoms
because of escalating antibiotic resistance.4,5 Due to
previous clinical trials that have shown positive outcomes for cranberry
preparations in preventing the incidence and recurrence of UTIs, cranberry is
seen as a potential alternative to low-dose antibiotics for UTI prevention.
The new clinical study included 185 women aged 65 or older who lived in 21
nursing homes in the New Haven, Connecticut, area. The women had to speak
English, had to have lived in the nursing home for at least four weeks, had to
have a life expectancy of more than one month, and had to be able to provide a
clean catch urine sample. Exclusion criteria included the following: the women could
not be on anti-infective therapy for recurrent UTIs, could not be undergoing
dialysis for end-stage renal disease, could not be receiving warfarin, could
not have a history of kidney stones, could not have a bladder catheter, or be
allergic to cranberry. In-service nurses were trained to collect appropriate
urine samples in order to have valid results. Urine samples were evaluated
every two months for the presence of bacteriuria (at least 100,000
colony-forming units of one or two types of bacteria per mL of urine) and
pyuria (any presence of white blood cells in the urine). 
From the 185 women that started the study, a follow-up after 12 months for the
presence of bacteriuria and pyuria was possible only for 90; patients were lost
due to protocol-unrelated deaths, transferal to hospice care, or development of
urinary incontinence. While urine analyses after four and six months showed
lower bacteriuria in the treatment group, the trend was reversed in the last
six months of the study, but without reaching statistical significance at any
time period. During the study period, a total of 350 UTIs were suspected, but
only 22 (10 in the treatment group and 12 in the placebo group) were confirmed
as symptomatic UTIs. The number of hospitalizations, presence of multi-drug
resistant bacteria, antibiotic treatments for suspected UTIs, and total
antimicrobials administered all trended in favor of the cranberry treatment;
however, the differences were not of statistical significance. No
treatment-related serious adverse events were observed. The frequency of
protocol-related non-serious adverse events, including altered mental status,
gastrointestinal discomfort, oral cavity issues, skin and soft tissue changes,
and weight loss, was similar in both groups.
The authors concluded that cranberry administration does not reduce the
occurrence of bacteriuria in older women living in nursing homes. However, 30%
of the subjects in both arms had asymptomatic bacteriuria at enrollment and
none were treated with antibiotics prior to starting the study. Cranberry has
not been consistently effective at reducing existing bacteriuria, as this could
be considered a “treatment” effect, which would not be an anticipated result
for cranberry. Various aspects were considered to be strengths of this study: the
use of a standardized cranberry product, compliance with the dosage regimen, and
use of objective criteria to evaluate treatment success. Listed shortcomings
included the inability to obtain urine samples from many women as the study
progressed due to subjects’ physical and mental impairments, the lack of an
anti-adhesion test (the interference of cranberry PACs with bacterial proteins,
inhibiting bacterial adherence to the mucous membranes of the urinary tract is one
of the mechanisms by which cranberry exerts its benefits rather than
bactericidal effects), and the inability to assess the efficacy of cranberry
supplementation in women with a history of recurrent UTIs.
Since
previous clinical trials have shown cranberry to be mainly effective in the
prevention of recurrent UTIs,6-10 the lack
of benefits in this study may not come as a surprise since only 1% of the
participants in the treatment group had three or more UTI episodes of in the 12
months prior to enrollment. While this clinical study suggests that there is no
benefit to using cranberry to prevent the presence of bacteriuria in this
particular population, a number of recent clinical trials carried out with
cranberry extracts provides evidence that cranberry has its place in the
therapeutic arsenal to prevent recurrent UTIs and radiation-induced cystitis.11
As such,
the suggestion to “move on from cranberries,” as stated by Lindsay E. Nicolle,
MD, professor at the Department of Internal Medicine and Medical Microbiology
at the University of Manitoba, in a JAMA
editorial12 based on the results of this study is not supported when scientific
evidence from all the published clinical trials is taken into account. Results
cannot be extrapolated beyond a negative effect of cranberry on prevention of
bacteriuria. This opinion was echoed by Kalpana Gupta, MD, Associate Professor of Medicine at Boston University School of
Medicine, who commented that she is “not ready to walk away from cranberries,”
and “some women with recurrent UTIs may still want to discuss cranberry treatment
with their doctors.”2
Concerns about the validity of the data were also raised in a statement
issued by the Cranberry Institute (CI), an organization dedicated to supporting
research on cranberries and promoting cranberry health benefits, and in a
letter written by Amy Howell, PhD, associate research scientist at the Philip
E. Marucci Center for Blueberry and Cranberry Research and Extension at Rutgers
University.13,14 Both the statement by the CI and Howell’s letter listed characteristics
of the clinical study design and results that do not support the conclusions
expressed in Nicolle’s editorial. Since this study was not designed to detect
the efficacy of cranberry on UTI prevention, conclusions about the benefits of
cranberry extracts to prevent recurrent UTIs should not be made based on the
results.
—Stefan Gafner,
PhD
References
1. Juthani-Mehta M, Van Ness PH, Bianco L,
et al. Effect of cranberry capsules on bacteriuria plus pyuria among older
women in nursing homes: A randomized clinical trial. JAMA. 2016.
2. Hoffman J. The Cure for
UTIs? It’s not Cranberries. New York
Times. October 27, 2016.
3. Juthani-Mehta M,
Datunashvili A, Tinetti M. Tests for urinary tract infection in nursing home
residents. JAMA. 2014;312(16):1687-1688.
4. Nicolle LE, Mayhew WJ,
Bryan L. Prospective randomized comparison of therapy and no therapy for
asymptomatic bacteriuria in institutionalized elderly women. The American Journal of Medicine. 1987;83(1):27-33.
5. Rowe TA, Juthani-Mehta M.
Diagnosis and management of urinary tract infection in older adults. Infect Dis Clin North Am. 2014;28(1):75-89.
6. Stothers L. A randomized
trial to evaluate effectiveness and cost effectiveness of naturopathic
cranberry products as prophylaxis against urinary tract infection in women. Can J Urol. 2002;9(3):1558-1562.
7. Walker EB, Barney DP,
Mickelsen JN, Walton RJ, Mickelsen Jr RA. Cranberry concentrate: UTI
prophylaxis. J Fam Pract. 1997;45(2):167-168.
8. Ferrara P, Romaniello L,
Vitelli O, Gatto A, Serva M, Cataldi L. Cranberry juice for the prevention of
recurrent urinary tract infections: A randomized controlled trial in children. Scand J Urol Nephrol. 2009;43(5):369-372.
9. Sengupta K, Alluri KV,
Golakoti T, et al. A Randomized, Double Blind, Controlled, Dose Dependent
Clinical Trial to Evaluate the Efficacy of a Proanthocyanidin Standardized
Whole Cranberry (Vaccinium macrocarpon)
Powder on Infections of the Urinary Tract. Curr
Bioact Comp. 2011;7(1):39-46.
10. Caljouw MAA, van den Hout
WB, Putter H, Achterberg WP, Cools HJM, Gussekloo J. Effectiveness of Cranberry
Capsules to Prevent Urinary Tract Infections in Vulnerable Older Persons: A
Double-Blind Randomized Placebo-Controlled Trial in Long-Term Care Facilities. J Am Geriatr Soc. 2014;62(1):103-110.
11. Bone K. Further evidence
for the clinical efficacy of cranberry: A brief review of recent clinical
trials. HerbalGram. 2016;112:29-33.
12. Nicolle LE. Cranberry for
prevention of urinary tract infection?: Time to move on. JAMA. 2016.
13. Efficacy of Cranberry
Products in Urinary Tract Health. 2016; http://cranberryinstitute.org/JAMA%20Response%20Statement%20-%20For%20CI%20Website.pdf. Accessed November 02, 2016.
14. Howell AB. Comments on JAMA
Study and Editorial on Cranberry and Bacteriuria. Chatsworth, NJ: Rutgers
University; 2016.
|