Issue:
112
Page: 46-59
Kratom: Medicine or Menace?
by Connor Yearsley
HerbalGram.
2016; American Botanical Council
In the United States, a proposed regulatory action on two
compounds found in the Southeast Asian herb kratom (Mitragyna speciosa,
Rubiaceae) has generated considerable public, professional, and media interest.
In a notice of intent published in the Federal Register on August 31, 2016, the
US Drug Enforcement Administration (DEA) announced the temporary listing of the
kratom alkaloids mitragynine (MG) and 7-hydroxymitragynine (7-OH-MG) in
Schedule I of the Controlled Substances Act (CSA) of 1970. The CSA defines
Schedule I controlled substances, which include heroin, LSD, and marijuana (Cannabis
spp., Cannabaceae), as “those that have a high potential for abuse, no
currently accepted medical use in treatment in the United States, and a lack of
accepted safety for use under medical supervision.”1-3
The temporary scheduling, which would have taken effect on
September 30, was “necessary to avoid an imminent hazard to the public safety,”
according to the DEA.1 But backlash from the public and members of Congress
prompted the DEA to announce on October 13 that it would withdraw its original
notice of intent and allow for a public comment period through December 1,
2016. The DEA also stated that it would receive from the US Food and Drug
Administration (FDA) a scientific and medical evaluation and scheduling
recommendation for the compounds.4,5
After the public comment period, the DEA could decide to
permanently place the compounds in a schedule of the CSA, which would require
an additional period for lawmakers and the public to comment, or it could
decide to move forward with the temporary scheduling that was originally
proposed, which would not require an additional comment period.4,5
The proposed temporary scheduling would have lasted for two
or three years. Under the CSA, a substance meeting the statutory requirements
for temporary scheduling may be placed only in Schedule I.1
The placement of the compounds in Schedule I, in effect,
would mean that possession and distribution of any preparations of kratom, a
plant that has shown the potential to help wean recovering addicts off heroin
and other addictive and dangerous opioids, would be illegal and could result in
criminal prosecution.6,7 Notably, cocaine and methamphetamine are currently
listed in Schedule II, meaning that, unlike Schedule I substances, physicians
can prescribe or administer these substances.3,8
Kratom is a tropical evergreen, broad-leafed tree native to
peninsular Thailand, southeastern Myanmar, Malaysia, Borneo, Sumatra, the
Philippines, and New Guinea. The herb is in the same family (Rubiaceae) as
other economically and medicinally important plants, including coffee (Coffea
arabica), gardenias (Gardenia spp.), and trees in the genus Cinchona (e.g., C.
officinalis and C. pubescens).9 Preparations of kratom leaves have been used
for centuries in Southeast Asia for a wide range of purposes, including as an
opium and alcohol substitute; to treat cough, diarrhea, and diabetes; to manage
pain, opioid withdrawal, and sexual dysfunction; and to stave off fatigue.6,10
In addition, the leaves have been applied to wounds and used as a vermifuge (an
agent that expels parasitic worms), and as a local anesthetic.9
Leaf preparations of the plant, including powders and teas,
act on the central nervous system. At low doses, they produce “cocaine-like” stimulant
effects, while higher doses produce “morphine-like” sedative and intoxicating effects.6
Therefore, some workers, such as seafarers, farmers, and rubber-tappers, in
southern Thailand, northern Malaysia, and elsewhere chew the fresh leaves to
increase work productivity and reduce fatigue during the day, and to relax
after work.9,11
Kratom, which started gaining popularity in the United
States within the last 15 years, has received increased media attention lately.
Although some people have successfully used kratom to recover from opioid and
alcohol addictions, there has been growing concern about the addictive
potential of kratom itself. The DEA notice repeatedly refers to kratom’s
potential for abuse.1
The DEA’s scheduling proposal comes in the midst of an
unprecedented opioid epidemic in the United States. For example, in 2012, there
were 12 states with more opioid prescriptions than residents. The ratio was the
largest in Alabama, where there were 142.9 opioid prescriptions per 100 people,
according to the Centers for Disease Control and Prevention (CDC).12 Even
worse, opioids, including both prescription pain relievers and heroin, were
involved in 28,647 deaths in the United States in 2014 (an average of 78 deaths
per day), more than any year on record. In addition, opioid overdoses
quadrupled between 2000 and 2014.13 In this context, it is obvious that
solutions are needed, but there is disagreement about whether kratom is helping
the problem or contributing to it.
Differing Perceptions of Kratom
At the time of the DEA’s August 31 notice of intent, six US
states (Alabama, Arkansas, Indiana, Tennessee, Vermont, and Wisconsin);
Washington, DC; and at least 15 countries, including Thailand, had banned
kratom. It had been included on the DEA’s “Drugs of Concern” list since 2005.1,9
After the notice, there was an outpouring of people who came to the defense of
the plant. Within two weeks, a petition on We the People
(petitions.whitehouse.gov) asking the White House to stop the scheduling had
garnered nearly 125,000 signatures (and, at press time for this article, more
than 143,000 signatures), surpassing the 100,000 necessary to receive a
response.14
In the days leading up to the originally proposed scheduling
date, 51 members of the House of Representatives, spurred by the Botanical
Education Alliance, an organization whose stated mission is to preserve plant
legality through education, formally requested that the DEA delay the
scheduling.15 Shortly thereafter, Senator Orrin Hatch (R–UT), the most senior
Republican senator, wrote a letter asking the DEA “to allow both for a public
comment period and sufficient time for the DEA to outline its evidentiary
standards to the Congress regarding the justification for this proposed action.”16
Days later, Senator Cory Booker (D–NJ), Senator Kirsten
Gillibrand (D–NY), and Senator Ron Wyden (D–OR) wrote an emphatic letter to DEA
Acting Commissioner Chuck Rosenberg in which they echoed Hatch’s requests. They
cited the eight-fold increase in US prison populations from the enforcement of “draconian
drug laws,” writing: “We should not, in haste and without adequate opportunity
for comment and analysis, place substances in categories that may be
inconsistent with their medical value and potential for abuse.”17
Anecdotal Evidence
After the DEA notice, many news articles told the stories of
people who claimed to have benefitted from kratom and who would personally be
affected by its placement in Schedule I. For example, one woman from Missouri
named Margo Burton had been taking two teaspoons of an unspecified preparation
of kratom every three hours to help her cope with pain caused by endometriosis,
a condition in which uterine tissue grows outside the uterus. “I need it so I’m
not hurting, so I can be a good mother,” Burton is quoted as saying. When she
heard about the DEA’s plan to ban kratom, she sobbed.18
Susan Ash, founder of the American Kratom Association (AKA),
a nonprofit that supports kratom users, started using kratom to manage pain
caused by Lyme disease that went undiagnosed for years. In 2008, her condition
became debilitating. “The pain was excruciating,” Ash is quoted as saying. “It
was in my joints. It would wake me up in the middle of the night. It would have
me in the emergency room.” Her doctors began prescribing drugs to treat the
symptoms of the undiagnosed disease, and then began prescribing more drugs to
treat the side effects of the other drugs.18,19
Ash was prescribed a cocktail of as many as 10 different
prescription drugs and soon began suffering serious neurological effects. She
was finally diagnosed with Lyme disease, but, by that point, she was addicted
to painkillers. In 2011, she entered treatment and successfully detoxed, but
she still felt chained to opioids.19 “Life couldn’t have been much worse at
that point. I was not leaving the house at all. I was only leaving the house to
see doctors,” she said. Then, someone suggested that she try kratom and,
although she was skeptical at first, she eventually did. “In a matter of two
weeks, I had the energy, I had the pain relief, and I had the depression and
anxiety relief I needed to become a productive member of society again. It was
such a stark difference and such an immediate change in my life.”19
In a video on YouTube, a US Army veteran, who says he
suffered from terrible foot and lower back pain and migraine headaches, talks
about his experience with kratom and his opinion of the DEA’s proposed
scheduling. “One of my best friends introduced me to this substance called
kratom,” he said. “I started taking it, and my pain went away…. I brew up some
tea leaves, let it steep for 40 minutes or whatnot, have a cup of tea, I feel
better.” Later in the video, he continued: “I’m not talking about snorting
cocaine, shooting up heroin. I’m not even talking about puffing a joint. I’m
talking about brewing some tea, having a sip, and feeling better — being able
to go for a run because my feet don’t kill me after six years in the army.”20
These are just some of the many anecdotal reports about the
potential benefits of kratom. There are hundreds of testimonials on YouTube and
elsewhere, some from military veterans using kratom to cope with post-traumatic
stress disorder (PTSD), some from people using it to manage fibromyalgia and
other painful conditions, and some from people using it to recover from
alcoholism.21 Testimonials like these and responses from members of Congress
played a part in convincing the DEA to withdraw its original notice of intent
and allow for public comment.
A Public Health Threat?
Still, some contend that kratom is dangerous. Dan Fabricant,
PhD, CEO and executive director of the Natural Products Association (NPA), was
the director of the Office of Dietary Supplement Programs at the FDA when the
administration first took actions against kratom as an unapproved new dietary
ingredient. In a recent NPA press release, he noted: “Kratom has been a public
health target for almost five years, and its surging growth in use and
availability is an unfortunate but real example of the federal government’s
unwillingness to use existing authorities to enforce the law. This [the DEA’s
scheduling] is a necessary and welcome step, but unless it is followed with
real enforcement and penalties for those who are selling it in coffee bars, on
the internet, and elsewhere, it will be toothless. Kratom is not an herbal
supplement: it is addictive, harmful, and worse, it may be contributing to [the
US's opioid] epidemic.”22
The original DEA notice stated that there have been numerous
deaths associated with kratom, beginning with a cluster of nine deaths in
Sweden between 2009 and 2010 that were linked to a product called “Krypton.”1
According to other sources, kratom-containing products sold under the name “Krypton”
were found to be adulterated with caffeine and synthetic O-desmethyltramadol (a
metabolite of the prescription opioid tramadol), but the DEA notice does not
mention this adulteration.6,9
According to the DEA notice, five other deaths related to
kratom exposure were subsequently reported in the scientific literature, and
autopsy/medical examiner reports for an additional sixteen deaths confirmed the
presence of MG and 7-OH-MG in biological samples. Of these 21 deaths, 15
occurred between 2014 and 2016.1
A toxicologist was hired by the AKA to review the 15 deaths
that occurred between 2014 and 2016, and in each case the toxicologist disputed
the notion that kratom toxicity was the cause of death.23 According to Ash,
many of these deaths involved other drugs, and some likely involved
pre-existing health conditions.
Adverse interactions have been reported involving kratom tea
taken with substances such as carisoprodol (a muscle relaxant), modafinil (a
wakefulness-promoting agent), propylhexedrine (a stimulant used as a nasal
decongestant), or jimson weed (Datura stramonium, Solanaceae; a tropane
alkaloid-containing plant with hallucinogenic and analgesic properties). In
addition, a fatal case in the United States (presumably counted among the
fatalities noted by the DEA) involved a mixture of kratom, fentanyl (a powerful
synthetic opioid analgesic), diphenhydramine (a sedating antihistamine), caffeine,
and morphine, which was mislabeled and illegally sold as an herbal product.6
Morphine-like Effects
MG and 7-OH-MG produce analgesic effects similar to those of
morphine, the prototypical opioid, and the DEA notice and other sources
classify them as opioids because of their binding affinity for the opioid
receptors.1
The term “opioid” combines “opium” with the suffix “-oid,” which
means “like” or “resembling” and often implies an incomplete or imperfect
resemblance to the preceding element. The term was originally proposed to
describe drugs that have actions similar to, but chemical structures different
from, morphine.24 The term “opioid” should also be distinguished from “opiate,”
which is a narrower term that refers to naturally occurring alkaloids found in
the opium poppy (Papaver somniferum, Papaveraceae), including morphine and
codeine.25
According to the book Kratom and Other Mitragynines (CRC
Press, 2015), substances are typically classified as opioids based on the
following criteria: binding affinity for one or more of the major subtypes of
opioid receptor, morphine-like in vivo effects (such as pain relief), miosis
(excessive constriction of the pupil), constipation, respiratory depression,
tolerance, cross-tolerance to a known opioid, development of dependence, and
similarity of chemical structure to morphine or another opioid.9 It has been
shown that MG and 7-OH-MG meet most of these criteria, at least to some degree.
However, David Kroll, PhD, a pharmacologist, member of the
American Botanical Council’s (ABC’s) Advisory Board, and medical writer who has
written articles about kratom for Scientific American and Forbes.com, said that
the pharmacological actions of MG and 7-OH-MG (see “In Depth: Botany and
Pharmacology of Kratom” section) more closely resemble those of buprenorphine
(a semisynthetic opioid with mixed opioid partial agonist/antagonist effects
and that is used to treat opioid addiction) than those of other, more common
opioids, such as morphine, hydrocodone, oxycodone, and heroin (email, October
16, 2016).
Kratom is one of a finite number of plants that have been
found to produce compounds that have an affinity for opioid receptors,
including P. somniferum; P. bracteatum, which produces thebaine, an opiate
precursor to a variety of semisynthetic opioids, such as buprenorphine26; P.
orientale, which also produces thebaine, in addition to oripavine, another
opiate precursor to several semisynthetic opioids27; Salvia divinorum (Lamiaceae),
which produces salvinorin A9; and Dalea purpurea (Fabaceae), which produces
pawhuskin A, B, and C.28
Respiratory Depression
Perhaps the most significant way in which MG and 7-OH-MG
differ from common opioids is that they have a much lower risk of producing
respiratory depression.21 (Notably, the misuse of the opioids fentanyl and
carfentanil, a fentanyl analog that is approximately 10,000 times more potent
than morphine, has resulted in an epidemic of overdose deaths caused by these
respiration-depressing effects.29) At lower doses, common opioids reduce the
amount of air passing into and out of the lungs in each respiratory cycle, and
therefore depress respiration. At higher doses, opioids further decrease
respiratory rate and impair respiratory rhythm. Opioid use also is associated
with rigidity of the muscles used during respiration and decreased activity of
these muscles during sleep.9 This respiratory depression can starve the brain
of oxygen and lead to permanent brain damage or death. The risk is heightened
when opioids are taken with other depressants, such as alcohol, antihistamines,
barbiturates, benzodiazepines, or general anesthetics.30
“It turns out mitragynine has a very low risk of respiratory
depression,” Kroll is quoted as saying. “It also appears that it’s very
difficult to at least get animals — get mice addicted to ‘mitra,’ either with
the herb or with the pure chemical.”21 In addition, at higher doses, kratom
induces vomiting, reportedly making it difficult to overdose.23
Kratom Use and Potential for Misuse
According to the European Monitoring Centre for Drugs and
Drug Addiction (EMCDDA), a few grams of dried kratom leaves produce
invigorating and euphoric effects within about 10 minutes, and these effects
last for about one to one-and-a-half hours. Kratom users report increased
alertness, sociability, and sometimes increased libido. Slight constriction of
the pupils and blushing may occur. In one of the few human clinical
experiments, a 50-mg oral dose of MG produced motor excitement, then giddiness,
loss of motor coordination, and tremors of the extremities and face.6
Larger doses of dried kratom leaves (10-25 g) may initially
cause sweating, dizziness, nausea, and dysphoria, but these effects are quickly
replaced with euphoria, calmness, and a dreamlike state that can last for up to
six hours. Miosis also occurs.6
Traditionally, when kratom is consumed as a tea, lemon juice
is often added to encourage extraction of the alkaloids in the plant. Sugar or
honey may be added to mask the bitterness of the tea. The dried leaves are also
sometimes smoked. The veins of the leaves are usually removed before
consumption, and salt may be added to prevent constipation. Kratom consumption
is sometimes followed by drinking warm water, coffee, tea, or palm sugar syrup.6
“With anything, there are dangers of using too much,” Walter
C. Prozialeck, PhD, professor of pharmacology at Midwestern University and
co-author of a review of the pharmacology of kratom, is quoted as saying.19 “But
the amount that a person has to take in to get any severe effects is ridiculously
high. You’re talking 10 to 15 grams of raw leaf. Most people who are using
kratom for pain management don’t take that much. Most people can’t take that
much.”
In addition, according to Prozialeck, kratom doesn’t produce
much of a psychoactive high in low to moderate doses. “After researching the
literature, I found that there were more positive aspects to kratom than there
were negative,” he is quoted as saying. “Additional studies are needed to
explore potential benefits of kratom. Also, work is needed to look at toxicity,
though.”19
The original DEA notice pointed to data from poison control
centers in the United States as evidence “that there is an increase in the
number of individuals abusing kratom.” Between 2000 and 2005, the American
Association of Poison Control Centers identified two exposures to kratom. In
the six-year period from January 2010 through December 2015, US poison centers
received 660 calls related to kratom exposure, and 428 (64.8%) of those
involved kratom being used with other substances, including ethanol,
benzodiazepines, narcotics, acetaminophen, and other botanicals.1 Compared to
the more than 3.1 million calls received by the US’s 55 poison centers in 2013
alone, calls involving kratom accounted for a tiny fraction.31
In addition, the DEA notice stated that it is especially
concerning that “users have turned to kratom as a replacement for other
opioids, such as heroin.”1 This is despite the fact that heroin was involved in
more than 8,200 deaths in the United States in 2013, and the fact that heroin
injection increases the risk of serious viral infections, including HIV and
hepatitis B and C, and bacterial infections of the skin, bloodstream, and
heart.32 Furthermore, methadone, a synthetic opioid that is sometimes used to
help wean recovering addicts off heroin, is involved in nearly 5,000 overdose
deaths per year.33 According to Kroll, buprenorphine (the pharmacological
actions of which, again, resemble those of MG and 7-OH-MG) has been replacing
methadone in opioid maintenance therapy for recovering opioid addicts. There is
concern among kratom proponents that if the DEA criminalizes kratom, it will
push some people back to abusing heroin and/or other opioids.23 Perhaps time
will tell.
Evidence suggests that kratom can be at least somewhat
addictive. Mark Swogger, PhD, an assistant professor of psychiatry at the
University of Rochester Medical Center and co-author of a qualitative analysis
of 161 firsthand descriptions of human kratom use, is quoted as saying: “I
think it’s pretty safe to say that kratom has at least some addiction
potential. The data is fairly strong on that, and our study also found that
people are reporting addiction. Overall, we found that it’s really mild
compared to [common] opioid addiction and it didn’t seem to last as long.”34
In addition, tolerance has been observed. New kratom users
typically need only a few leaves to feel an impact, but heavy users may need to
chew the leaves between three and 10 times per day, and some users find that,
over time, they need to increase the number of leaves chewed to between 10 and
30, or more, per day.9 Furthermore, mice treated with 7-OH-MG developed
tolerance, cross-tolerance to morphine, and withdrawal symptoms that could be
brought on by administration of naloxone, a semisynthetic opioid receptor
antagonist (i.e., an inhibitor of receptor activity) that is used to reverse
the effects of opioids in cases of overdose or postoperative sedation.6
Regular kratom users may also become dependent. Human
withdrawal symptoms are fairly mild and usually subside within a week. These
symptoms include anxiety, restlessness, runny nose, muscle pain, weakness,
lethargy, nausea, sweating, craving, jerky movements of the limbs, sleep
disturbances, and sometimes hallucination.6
Prior Regulatory Actions
Before the DEA’s notice of intent, kratom qualified as a
dietary ingredient under the Federal Food, Drug, and Cosmetic Act (FDCA) of
1938 that could be used in dietary supplement products. However, under the
Dietary Supplement Health and Education Act (DSHEA) of 1994, the FDA considers
it a new dietary ingredient (NDI) because there is no information demonstrating
that it was marketed as a dietary ingredient in the United States before
October 15, 1994. If an ingredient is considered “new,” then companies must
meet certain additional regulatory requirements before using the ingredient in
a supplement product.
The FDA did not believe that these regulatory requirements
had been satisfied by any company that was marketing and selling kratom, and
thus considered kratom and kratom-containing dietary supplements and bulk
dietary ingredients to be adulterated under the FDCA. In February 2014, the FDA
issued an import alert notifying field personnel that they could detain
kratom-containing products listed in the alert without physical inspection.35
In a separate alert, the FDA announced that other listed kratom products could
be detained without physical inspection because these products were considered
unapproved and/or misbranded drugs.36 In these cases, importers and marketers
were making unauthorized disease-treatment claims for their products. Between
2014 and the time of the DEA notice, products from 121 firms had been added to
the two FDA import alerts.1
In September 2014, US Marshals, at the request of the FDA,
seized more than 25,000 pounds of raw kratom material worth more than $5
million.37 In January 2016, US Marshals, again at the request of the FDA,
seized nearly 90,000 bottles of dietary supplements labeled as containing kratom.38
And again, in August 2016, US Marshals, at the request of the FDA, seized 100
cases of products labeled as containing kratom.39
Between February 2014 and July 2016, more than 55,000
kilograms (121,254 pounds) of kratom material was encountered at various ports
of entry in the United States. In addition, at the time of the DEA notice, more
than 57,000 kilograms (125,663 pounds) of kratom material offered for import at
numerous ports of entry between 2014 and 2016 was awaiting an admissibility
decision by the FDA. At the time of the DEA notice, the amount of kratom that
had been seized or that was awaiting an admissibility decision was estimated to
be enough to produce more than 12 million doses of kratom. According to the
DEA, “such alarming quantities create an imminent public health and safety
threat.”1
The DEA’s scheduling proposal came as a surprise to some. “While
I’m not surprised that the FDA began to seize kratom as an unapproved drug…, I
was surprised by the DEA’s intent to place two of the alkaloids in Schedule I,”
Kroll wrote (email, September 19, 2016). “But I have to admit that it took me
writing an article about kratom and getting reader comments before I realized
people were overwhelmingly using the herb medically and not as a recreational psychotropic.”
Impact on Research
Kroll also mentioned that two important kratom studies were
only recently published: one by Kruegel et al. (from Columbia University) that
was published in May 2016 in the Journal of the American Chemical Society40 and
one by Váradi et al. (from Memorial Sloan Kettering Cancer Center) that was
published in August 2016 in the Journal of Medicinal Chemistry.41 “So the DEA
may not have been aware of the firm distinctions between Mitragyna speciosa
alkaloids and strong, full agonist opioids [a full agonist binds to and
activates a receptor, producing full activity at that receptor],” Kroll wrote. “What
this tells me is that the DEA rushed to judgment based on the weak adverse
[event] report record of the herb and/or its adulterants without fully
investigating that its compounds were pharmacologically distinct from strong
opioid agonists [e.g., morphine].”
Ash of the AKA is quoted as saying she “really believed that
because of the progress medical marijuana has made through the states that the
federal government was going to leave kratom alone and leave it to the states
to decide whether it was appropriate to be legal.”42
It is not entirely clear how the scheduling would impact
research on kratom. Researchers will have to apply to the DEA for a Schedule I
research license, which requires a fairly stringent collection of documentation
and security protocols that can take time to implement, up to a year or more,
wrote Kroll. “The researchers I’ve spoken to are more concerned about the
availability of research amounts of raw plant material, since import
restrictions on Schedule I substances are quite ornery,” he wrote.
DEA spokesperson Russ Baer is quoted as saying, “As is the
case with any controlled substance, the DEA will implement aggregate production
quotas for kratom and make available an adequate and uninterrupted supply of
research-grade material to accommodate valid scientists and researchers.”43
It is possible this may be done through a federal supply
contract similar to the marijuana farm at the University of Mississippi, which,
until recently, supplied all of the medical cannabis used for DEA-approved
research.44
According to Jahan Marcu, PhD, chief scientific officer for
Americans for Safe Access, a medical cannabis advocacy organization, “it is
unclear how long it would take the DEA to supply kratom, since it can take 20
years for a tree to reach maturity. A federal supply of kratom, produced in the
US, is 20 years away, leaving our [kratom] researchers to whither on the vine
because they do not have access to their research tools” (email, October 13,
2016).
Schedule I study restrictions on kratom would undoubtedly “stall
the scientific study of the herb at a time when our understanding of its molecular
pharmacology has never been more advanced and promising,” Kroll wrote.
Additionally, he thinks the scheduling will hinder the study of semisynthetic
analogs of the M. speciosa alkaloids that could lead to new FDA-approved drugs
for pain and/or recovery from opioid and alcohol dependence.
In Depth: Botany and Pharmacology of Kratom
Kratom grows in swamps and damp valley areas that are rich
with humus, and forms “dense stands in the new alluvial substrate of ox-bow
lakes and low muddy river banks that are frequently inundated.”9 The species is
said to be a common riverside pioneer (i.e., a species that is the first to
colonize previously disrupted or damaged ecosystems).
According to one source, the tree can grow to 4-16 meters
(13-52 feet) tall with a spread of more than 15 feet.6,45 According to Kratom
and Other Mitragynines, it can grow to 25 meters (82 feet) in height and two to
three feet in diameter. The trunk is usually straight. The outer bark is smooth
and gray, and the inner bark is pinkish.9 The leaves are oval or
ovate-lanceolate and dark green.6 They are 14-20 centimeters long and 7-12
centimeters wide.9 The veins of the leaves are either greenish-white or red.
Leaves with greenish-white veins are said to be more potent. The average weight
of a fresh leaf is about 1.7 grams, while the average weight of a dried leaf is
about 0.43 grams. The tree produces yellow and globular flowers that can bear
up to 120 florets. The fruit is a capsule that contains several small, flat
seeds.6
Alkaloid Chemistry and Composition
The tree contains more than 40 structurally related
alkaloids, in addition to several flavonoids, saponins, polyphenols, and
glycosides. Kratom is the only species known to produce the indole alkaloids MG
and 7-OH-MG, two of the main psychoactive components in the plant.6 At least
three other alkaloids found in kratom (speciogynine, paynantheine, and
speciociliatine) have been shown to have some opioid receptor affinity.46
The chemical profile of kratom varies depending on several
factors: the variety and age of the plant, the environment, and the time of
harvest. The total alkaloid concentration in dried leaves typically ranges from
0.5% to 1.5%.6
MG is structurally similar to yohimbine (a compound derived
from the African tree yohimbe [Pausinystalia johimbe, Rubiaceae]),10 and it is
typically the most abundant alkaloid in the leaves,9 although it has also
reportedly been found in the fruits and stembark of kratom.47 MG was first
isolated in 1921, and its structure was determined in 1965.9
The amount of MG that kratom yields depends on geography and
the maturity of the leaves.9 For example, MG accounted for 66% of the crude
base of alkaloids extracted from young leaves of a specimen from Thailand,
while the compound accounted for only 12% of the alkaloids extracted from
mature leaves of a specimen from Malaysia.47 It is possible that, in this case,
geography, not leaf maturity, accounted for the difference, since, according to
Kratom and Other Mitragynines, MG is typically much more abundant in older
plants than younger ones, and much more abundant in Thai plants than Malaysian
ones. Interestingly, the predominant alkaloid found in a kratom specimen grown
at the University of Mississippi was the oxindole-type mitraphylline (at 45% of
the total alkaloids), not MG.9 Mitraphylline is also found in the bark of cat’s
claw (Uncaria tomentosa, Rubiaceae).48
7-OH-MG is a minor alkaloidal constituent of kratom. It
accounted for just 2% of the crude base of alkaloids extracted from young
leaves of a specimen from Thailand. A 2004 study using guinea pigs showed that
7-OH-MG was almost 50-fold more potent than MG and more than 10-fold more
potent than morphine.47 Another study using guinea pigs, however, showed that
7-OH-MG was 30-fold more potent than MG and 17-fold more potent than morphine.46
It is thought that 7-OH-MG is more potent than morphine because it is more
lipophilic (i.e., able to combine with or dissolve in fats) than morphine and
distributes more quickly across the blood-brain barrier, a diffusion barrier
that impedes the influx of most compounds from the blood into the brain.9,49
However, 7-OH-MG is less lipophilic than MG, and it is thought that it is more
potent than MG because of tighter receptor binding to the mu-opioid receptors
(MORs), which is associated with 7-OH-MG’s hydroxyl group (-OH) at the C7
position, a structural feature not present in MG.9,40
MG and mitraphylline have also been shown to be able
to diffuse across the blood-brain barrier in vitro. In addition, MG and 7-OH-MG
were found by one study to be unstable in simulated gastric fluid (which could
account for why some of the 7-OH-MG [23%] was converted to MG), but both were
found to be stable in simulated intestinal fluid.48 MG is not soluble in water,
but it is soluble in conventional organic solvents (i.e., solvents that contain
carbon atoms).6
Receptor Activity and Mechanisms of Action
According to the study conducted by researchers at Columbia
University, both MG and 7-OH-MG are partial agonists of the MORs, and MG was
shown to have about 34% of the maximal effect of a full agonist. This study was
conducted using human kidney cells that had been genetically modified to
express the human versions of each opioid receptor subtype. MORs are located in
the brain, spinal cord, and gastrointestinal tract, and MOR agonists (like
morphine) are the “gold standard” of pain therapy. But, in addition to
producing analgesia, MOR activation can produce serious adverse side effects,
including constipation, sedation, nausea, itching, and, as previously
mentioned, respiratory depression. In addition, the euphoria produced by MOR
agonists makes them widely subject to misuse.40
Kroll proposed three explanations for why MG and 7-OH-MG
cause less-to-no respiratory depression, compared with other MOR agonists. “First,
they are partial agonists at the MORs, meaning that the maximal effect is lower
than the maximal effect of a full agonist like morphine,” he wrote. “What this
means is that no matter how much MG or 7-OH-MG you put in the system, you’ll
never get to the same effect as the maximum effect of morphine.”
“Second, the Mitragyna speciosa alkaloids all appear to be ‘biased’
toward the G-protein signaling pathway and away from the beta-arrestin-2
pathway,” Kroll continued. “This is a relatively new and often confusing
concept, even to some pharmacologists. When a receptor sitting on the cell
surface is bound by a drug, it can either do nothing (as with a blocker, or
antagonist), or it can transduce a signal to the inside of the cell that
triggers a cascade of events. MORs can signal through a so-called G-protein
and/or the beta-arrestin-2 protein. Beta-arrestin-2 seems, at least in part, to
mediate respiratory depression (as well as tolerance, accounting for why
patients and addicts all require progressively more opioids over time to
produce the same effect).”
According to Kroll, a possible third reason “is that MG and
7-OH-MG are both antagonists at kappa-opioid receptors [KORs], albeit with less
potency than as partial MOR agonists. The overall effect is that you can get
painkilling approaching that of morphine with much less respiratory depression.”
KOR antagonists, such as MG and 7-OH-MG, have shown the
potential to help promote stress resilience, which may help treat certain types
of anxiety, depression, and addiction disorders, all of which are exacerbated
by hypersensitivity to stress.50 The Columbia University study also showed that
MG and 7-OH-MG are antagonists of the delta-opioid receptors (DORs).40 Animal
studies suggest that DORs control rewarding or addictive properties of drugs
that act on the MORs or other non-opioid receptor sites. Therefore, DOR
antagonists may have the ability to block morphine reward and tolerance.51
Interestingly, the Thai strain of kratom used by the
Columbia University researchers yielded only trace quantities of 7-OH-MG that
were too small to isolate. “Therefore,” the researchers wrote, “it is doubtful
that this alkaloid is a universal constituent of all Mitragyna speciosa preparations
and is unlikely to generally account for the psychoactive properties of this
plant.” They were, however, able to prepare 7-OH-MG through photochemical
oxidation of MG, which, according to Kroll, indicates that “growing and storage
conditions may dramatically affect the overall potency of the botanical
material.”40
In addition, the study found that paynantheine,
speciogynine, and speciociliatine (which, together, accounted for a percentage
of the total extracted alkaloids that was approximately equal to the percentage
accounted for by MG) all exhibited antagonist activity at the MORs that competed
with the agonist activity of MG. The researchers, therefore, concluded that “the
gross psychoactive effects of crude plant material are likely to represent a
complex interplay of competing agonist and antagonist effects at the opioid
receptors.”40
Kratom’s unusual and paradoxical stimulant/sedative effects
are not fully understood. “Some opioids have a paradoxical stimulating effect
in some patients, particularly in elderly folks,” Kroll wrote. “But the Mitragyna
speciosa alkaloids have some other receptor effects (e.g., alpha-2-adrenergic)
that may or may not be relevant for the amounts of kratom people consume. From
anecdotes, the [stimulating] effect does sound like it’s real but it hasn’t
been systematically studied in humans or attributed to a specific compound or
neuroreceptor system.”
One guinea pig study showed that MG may produce analgesic
effects through the blockade of neuronal calcium ion (Ca2+) channels.52 And
another source suggests that MG’s analgesic effects may involve the activation of
serotonergic and noradrenergic pathways that descend down the spinal cord. In
addition, kratom seems to have anti-inflammatory properties.10
Conclusion
Kratom is a complicated plant that is not fully understood,
either by the scientific community or by the global community. It is likely
that language has played a part in shaping perceptions about kratom, with some
sources referring to it as an opium “substitute” and other sources referring to
it as an opium “remedy.”9 Different perceptions of the plant have led some to
celebrate it for its medicinal potential and others to malign it for its abuse
potential.
At a time when the United States needs safer alternatives to
opioids more than ever, the DEA’s placement of the kratom alkaloids in Schedule
I would force those who were successfully using the plant for pain management,
opioid withdrawal, and other therapeutic purposes to become criminals, seek
alternatives that may be more dangerous, or simply do without. Detractors point
to the fact that kratom users may become addicted to, dependent on, and
tolerant of kratom over time. Proponents emphasize that the kratom alkaloids
produce less constipation and, more importantly, less-to-no respiratory
depression, compared to other common opioids.
However, proponents, and even some detractors, agree that
more research is needed, on both the potential benefits and the potential
dangers of kratom. DEA scheduling would make this research more difficult.
“I think that the best kratom researchers should get
together and write a couple of clinical trial protocols to the National Center
for Complementary and Integrative Health (NCCIH) to investigate a
well-characterized, analytical and GMP[good manufacturing practice]-verified
kratom product to investigate pharmacokinetics of each compound and metabolite,
and efficacy in pain and substance dependence recovery, while also assessing
adverse effects, including dependence on the kratom itself,” Kroll wrote.
As far as the individual compounds, Kroll believes that MG,
7-OH-MG, the fermentation product mitragynine pseudoindoxyl, and semisynthetic
analogs of each should be investigated as single-entity drugs. “But the
semisynthetic analogs will likely be required, not just for intellectual
property purposes, but for improved half-life and dosage formulation,” Kroll
wrote. “Users have told me they need to dose with kratom tea up to four or five
times in a day, and there is some published data that MG’s half-life [i.e., the
time it takes for half of the administered amount to be eliminated from the
bloodstream] is on the order of an hour.”
Though according to some it is not legally realistic to
expect kratom to remain unregulated, there is interest within the scientific
community about the potential for new therapeutics derived from the plant
(either single compounds or whole-plant preparations) to become safer and
better pain-relievers and opioid recovery aids. “At a time when the opioid
dependence issue is at its greatest national awareness,” Kroll wrote, “I think
we need any tool — pharmacological, psychological, [mindful] meditation, yoga,
etc. — that can relieve people of the burden, pain, and potential lethality of
substance dependence.”
Sidebar: Nomenclature and Taxonomy of Kratom
Mitragyna is a small genus that, depending on the taxonomic
treatment, includes seven to 10 species. (A taxonomic treatment is a
publication, or a section of a publication, that documents the features and/or
distributions of a related group of organisms [i.e., a taxon] in ways that
adhere to highly formalized conventions.54) According to one treatment, four Mitragyna
species are found in Africa, while six are found in South and Southeast Asia.
The Asian species are distributed between India and New Guinea.9
The Dutch botanist Pieter Willem Korthals (1807-1892) first
described the genus. As a member of the Commission for Natural Sciences of the
Dutch East India Company from 1830 to 1837, Korthals made important botanical
discoveries and collections in the Malay Archipelago.9 He named the genus Mitragyna
because he thought the leaves and stigmas of the flowers of one of the
specimens he observed resembled the shape of a bishop’s mitre.6 In 1839,
Korthals published the genus and the species name M. speciosa in the same
publication, but he didn’t include a botanical description of M. speciosa, and
that name is therefore considered a nomen nudum (a “naked name”). In 1842,
Korthals transferred the species to the genus Stephegyne. Various authors
subsequently renamed the species Nauclea korthalsii, then Nauclea luzoniensis,
then Nauclea speciosa, before British naturalist George Haviland set the
current accepted species name as M. speciosa in 1897.9
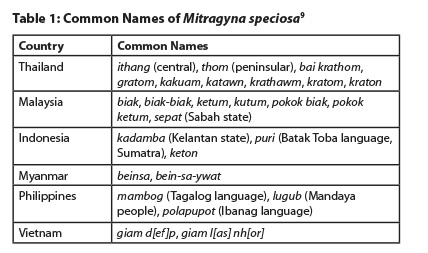
The common name “kratom” originates from Thailand,9 but the
plant has many common names (see Table 1). According to one source, “kratom” is
likely derived from the Sanskrit kadam, a name that refers to Neolamarckia
cadamba (Rubiaceae), a widespread tree that is sacred in Hinduism. Similar
names are used for various related tree species in the region.9
Sidebar: Kratom in Thailand
Perhaps nowhere in the world does kratom have a longer and
more interesting history than in Thailand. As in some other Southeast Asian countries,
there are potentially toxic, kratom-containing admixtures used in Thailand, and
various socioeconomic and political factors contribute to the perception of
kratom misuse. Some of these factors may have some relevance to the current
kratom debate in the United States.
In Thailand, chewing kratom leaves is a tradition that has
been practiced for centuries, especially on the southern peninsula where the
tree is more commonly found. According to one source, “In southern Thailand,
traditional kratom use is not perceived as ‘drug use’ and does not lead to
stigmatization or discrimination of users. Kratom is generally part of a way of
life in the south, closely embedded in traditions and customs such as local
ceremonies, traditional cultural performances, and teashops, as well as in
agricultural and manual labor in the context of rubber plantations and
seafaring.”53
In some districts in southern Thailand, as much as 70% of
the male population uses kratom on a daily basis (as of 2011), and many people
consider it similar to drinking coffee. Some southern provinces, especially
Pattani, Yala, and Narathiwat, are predominantly made up of Muslims who,
because of the dictates of Islam, cannot consume alcohol. Kratom is an
alternative that is not prohibited by the clergy, but it is controlled by the
government.53
Kratom was banned in Thailand under the Kratom Act of 1943.
Leading up to the ban, the Thai government had started levying taxes on opium
users and retailers. Because opium started becoming more expensive, many users
switched to kratom to help manage opium withdrawal. With the launch of the
Pacific War (which debatably began in December 1941 when Japan invaded Thailand
and attacked British possessions in the Pacific) and decreasing opium revenues,
the Thai government took action to eliminate competition in the opium trade.53
In 1943, a government official was quoted as saying: “Taxes
for opium are high while kratom is currently not being taxed. With the increase
of those taxes, people are starting to use kratom instead and this has had a
visible impact on our government’s income.”53
 After World War II, the Kratom Act was not aggressively
enforced, and kratom could be grown in moderation and consumed openly. In 1979,
kratom was included in the least restrictive and punitive schedule of the Thai
Narcotics Act. In the early 2000s, coinciding with a crackdown on illegal drugs
that was initiated by the Thai government, the number of seizures and arrests
related to kratom increased greatly. Shortly thereafter, in the mid-2000s, a
kratom-containing cocktail called “4x100” started being used by some young
people.53 The cocktail involves boiling kratom leaves (15 to 100 at a time) to
produce a tea, which is mixed with codeine- or diphenhydramine-containing cough
syrup, a soft drink (usually Coca-Cola), and ice cubes.9,53 Typically, the
cocktail is prepared twice or more per day, depending on the availability and
cost of the ingredients. 4x100 users are typically subject to some community
discrimination, though not as much as yaba (methamphetamine) or heroin users.53
There have been concerns about reports of the cocktail being
laced with additives “such as benzodiazepines, powder from fluorescent tubes,
powdered mosquito coils, road paint, pesticides, ashes from dead bodies, and
other substances found in the local environment to ‘enhance’ the effect of the
cocktail.” Apparently, little evidence to substantiate these claims has been
found, and some contend these are exaggerations meant to vilify those who
consume the cocktail, again, typically young people. One 4x100 user was quoted
as saying: “We want to get high, not kill ourselves!”53
Because of these reports, however, authorities, with the
stated intent of protecting young people, have been instructed to eradicate
kratom trees and actively look for kratom and 4x100 users in certain
communities (as of 2011). Beginning in the mid-2000s, several eradication
campaigns in the southern provinces led to large numbers of kratom trees being
cut down, either by law enforcement or by community groups (whether voluntarily
or not). In Pattani, Yala, and Narathiwat provinces, few kratom trees are left
in the wild. Authorities in Satun, Surat Thani, and Trang provinces are more
lenient and tolerate a few trees in the community and up to one tree per
household (as of 2011).53
According to one source, efforts to control kratom between
the early 2000s and 2011 did little good. Kratom is still popular in the
southern provinces and around Bangkok, though not among women (who usually
prefer to chew betel nut [Areca catechu, Arecaceae] instead). The traditional
chewers (as opposed to the 4x100 users) often own the land where kratom grows
and are, therefore, usually the ones targeted by eradication campaigns. Younger
4x100 users sometimes resort to stealing from trees in the community, which has
led some traditional chewers to set up barbed wire and other protection
mechanisms around kratom trees. In addition, efforts to limit 4x100 use has
almost exclusively focused on kratom, instead of trying to control cough syrup
and benzodiazepines, the most potentially harmful components of the cocktail.53
Although kratom is technically illegal in Thailand, law
enforcement has been uneven and many people continue to view kratom as a
traditional medicine. According to some, kratom should be decriminalized, and
community leaders should be empowered to control production and consumption of
kratom. In addition, some argue that concerns surrounding 4x100 use have little
to nothing to do with kratom.53
References
- Schedules of Controlled Substances: Temporary Placement of Mitragynine and 7-Hydroxymitragynine Into Schedule I. The Federal Register. Available at: www.federalregister.gov/documents/2016/08/31/2016-20803/schedules-of-controlled-substances-temporary-placement-of-mitragynine-and-7-hydroxymitragynine-into. Accessed September 14, 2016.
- Part 1308.11 Schedule I. Drug Enforcement Administration website. Available at: www.deadiversion.usdoj.gov/21cfr/cfr/1308/1308_11.htm. Accessed September 14, 2016.
- Controlled Substances Act. Food and Drug Administration website. Available at: www.fda.gov/regulatoryinformation/legislation/ucm148726.htm. Accessed September 15, 2016.
- Withdrawal of Notice of Intent to Temporarily Place Mitragynine and 7-Hydroxymitragynine Into Schedule I. The Federal Register. Available at: www.federalregister.gov/documents/2016/10/13/2016-24659/withdrawal-of-notice-of-intent-to-temporarily-place-mitragynine-and-7-hydroxymitragynine-into. Accessed October 13, 2016.
- Ingraham C. The DEA is withdrawing a proposal to ban another plant after the internet got really mad. The Washington Post website. October 12, 2016. Available at: www.washingtonpost.com/news/wonk/wp/2016/10/12/the-dea-is-reversing-its-insane-decision-to-ban-the-opiate-like-plant-kratom-for-now. Accessed October 18, 2016.
- Kratom (Mitragyna speciosa) drug profile. European Monitoring Centre for Drugs and Drug Addiction website. Available at: www.emcdda.europa.eu/publications/drug-profiles/kratom.
- The Controlled Substances Act (CSA): Overview. FindLaw website. Available at: http://criminal.findlaw.com/criminal-charges/controlled-substances-act-csa-overview.html. Accessed September 15, 2016.
- Part 1308.12 Schedule II. Drug Enforcement Administration website. Available at: www.deadiversion.usdoj.gov/21cfr/cfr/1308/1308_12.htm. Accessed September 14, 2016.
- Raffa RB, ed. Kratom and Other Mitragynines: The Chemistry and Pharmacology of Opioids from a Non-Opium Source. Boca Raton, FL: CRC Press; 2015.
- Prozialeck WC, Jivan JK, Andurkar. Pharmacology of kratom: An emerging botanical agent with stimulant, analgesic and opioid-like effects. J Am Osteopath Assoc. 2012;112(12):792-799. Available at: http://jaoa.org/article.aspx?articleid=2094342. Accessed September 14, 2016.
- Cinosi E, Martinotti G, Simonato P. Following “the roots” of kratom (Mitragyna speciosa): The evolution of an enhancer from a traditional use to increase work and productivity in Southeast Asia to a recreational psychoactive drug in western countries. Biomed Res Int. 2015;2015:968786. doi: 10.1155/2015/968786.
- Paulozzi LJ, Mack KA, Hockenberry JM. Vital Signs: Variation Among States in Prescribing Opioid Pain Relievers and Benzodiazepines — United States, 2012. CDC website. Available at: www.cdc.gov/mmwr/preview/mmwrhtml/mm6326a2.htm. Accessed September 14, 2016.
- Injury Prevention and Control: Opioid Overdose. CDC website. Available at: www.cdc.gov/drugoverdose/data/statedeaths.html. Accessed September 14, 2016.
- Please do not make Kratom a Schedule I Substance. White House website.
Available at: http://petitions.whitehouse.gov/petition/please-do-not-make-kratom-schedule-i-substance. Accessed September 30, 2016.
- Ault A. Congress Members Call for Halt on DEA Kratom Ban. Medscape website. September 28, 2016. Available at: www.medscape.com/viewarticle/869402. Accessed September 30, 2016.
- DiSalvo D. Kratom Has the Senate’s Attention, and the DEA’s Schedule I Date May Shift. Forbes website. September 29, 2016. Available at: www.forbes.com/sites/daviddisalvo/2016/09/29/kratom-now-has-the-senates-attention-and-the-deas-schedule-i-date-may-shift. Accessed September 30, 2016.
- Kroll D. DEA Delays Kratom Ban, More Senators Object to Process and “Unintended Consequences.” Forbes website. September 30, 2016. Available at: www.forbes.com/sites/davidkroll/2016/09/30/dea-delays-kratom-ban-more-senators-object-to-process-and-unintended-consequences. Accessed October 18, 2016.
- Boodman E. Hidden Network of Kratom Devotees Tries to Keep the Supplement Safe — and Legal. Stat News website. September 2, 2016. Available at: www.statnews.com/2016/09/02/kratom-devotees-fight-for-supplement/. Accessed September 15, 2016.
- Wing N. Some Say Kratom is a Solution to Opioid Addiction. Not if Drug Warriors Ban It First. Huffington Post website. March 3, 2016. Available at: www.huffingtonpost.com/entry/kratom-ban-drug-policy_us_56c38a87e4b0c3c55052ee3f. Accessed September 19, 2016.
- Soldier of the Year Speaks Out on Soldiers for Change on Kratom. YouTube website. September 2, 2016. Available at: www.youtube.com/watch?v=7VwKcTH2nik. Accessed September 19, 2016.
- Silverman L. Kratom Advocates Speak Out Against Proposed Government Ban. NPR website. September 12, 2016. Available at: www.npr.org/sections/health-shots/2016/09/12/493295493/kratom-advocates-speak-out-against-proposed-government-ban. Accessed September 16, 2016.
- DEA Kratom Change “Toothless” Without United States Government Enforcement, Says NPA [press release]. Washington, DC: Natural Products Association; August 31, 2016. Available at: www.npainfo.org/App_Themes/NPA/docs/press/PressReleases/Kratom%20Classification.pdf. Accessed September 19, 2016.
- Nelson S. DEA’s Sudden ‘Herbal Heroin’ Ban Triggers Stiff Resistance from Kratom Community. US News website. September 1, 2016. Available at: www.usnews.com/news/articles/2016-09-01/deas-sudden-herbal-heroin-ban-triggers-stiff-resistance-from-kratom-community. Accessed September 19, 2016.
- Opium and opioids: a brief history. Available at: www.scielo.br/scielo.php?pid=S0034-70942005000100015&script=sci_arttext&tlng=en. Accessed September 21, 2016.
- Levine B, ed. Principles of Forensic Toxicology. Washington, DC: AACC Press; 2003.
- Seddigh M, Jolliff GD, Calhoun W, Crane JM. Papaver bracteatum, potential commercial source of codeine. Economic Botany. 1982;36(4):433-441.
- Shafiee A, Lalezari I, Nasseri-Nouri P, Asgharian R. Alkaloids of Papaver orientale and Papaver pseudo-orientale. Journal of Pharmaceutical Sciences. 1975;64(9):1570-1572. doi: 10.1002/jps.2600640937.
- Belofsky G, French AN, Wallace DR, Dodson SL. New geranyl stilbenes from Dalea purpurea with in vitro opioid receptor affinity. J Nat Prod. 2004;67(1):26-30.
- Emerging Trends and Alerts. National Institute on Drug Abuse website. Available at: www.drugabuse.gov/drugs-abuse/emerging-trends-alerts. Accessed October 18, 2016.
- What Are the Possible Consequences of Opioid Use and Abuse? Drug Abuse website. Available at: www.drugabuse.gov/publications/research-reports/prescription-drugs/opioids/what-are-possible-consequences-opioid-use-abuse. Accessed September 22, 2016.
- American Association of Poison Control Centers. AAPCC website. Available at: www.aapcc.org/. Accessed September 26, 2016.
- Today’s Heroin Epidemic. CDC website. Available at: www.cdc.gov/vitalsigns/heroin/. Accessed September 26, 2016.
- Prescription Painkiller Overdoses. CDC website. Available at: www.cdc.gov/vitalsigns/methadoneoverdoses/. Accessed September 26, 2016.
- Szalavitz M. Why Banning the Controversial Painkiller Kratom Could Be Bad News for America’s Heroin Addicts. Vice website. January 20, 2016. Available at: www.vice.com/read/why-banning-the-controversial-painkiller-kratom-could-be-bad-news-for-americas-heroin-addicts. Accessed September 26, 2016.
- Import Alert 54-15. Food and Drug Administration website. Available at: www.accessdata.fda.gov/cms_ia/importalert_190.html. Accessed September 28, 2016.
- US Marshals seize botanical substances kratom from southern California facility [press release]. Silver Spring, MD: Food and Drug Administration; September 25, 2014. Available at: www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm416318.htm. Accessed September 26, 2016.
- US Marshals seize dietary supplements containing kratom [press release]. Silver Spring, MD: Food and Drug Administration; January 6, 2016. Available at: www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm480344.htm. Accessed September 26, 2016.
- Kratom seized in California by US Marshals Service [press release]. Silver Spring, MD: Food and Drug Administration; August 4, 2016. Available at: www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm515085.htm. Accessed September 26, 2016.
- Kruegel AC, Gassaway MM, Kapoor A, et al. Synthetic and receptor signaling explorations of the Mitragyna alkaloids: Mitragynine as an atypical molecular framework for opioid receptor modulators. J Am Chem Soc. 2016;138(21):6754-64. doi: 10.1021/jacs.6b00360.
- Varadi A, Marrone GF, Palmer TC, et al. Mitragynine/corynantheidine pseudoindoxyls as opioid analgesics with mu agonism and delta antagonism, which do not recruit beta-arrestin-2. J Med Chem. 2016;59(18):8381-8397. doi: 10.1021/acs.jmedchem.6b00748.
- Wing N. Feds Declare War on Herb Touted as a Solution to Opioid Addiction. Huffington Post website. August 30, 2016. Available at: www.huffingtonpost.com/entry/dea-kratom-schedule-i_us_57c5c263e4b0cdfc5ac98b83. Accessed September 21, 2016.
- Boodman E. Kratom Ban Will Hinder Studies of the Plant for Treating Pain or Addiction, Researchers Say. Stat News website. September 8, 2016. Available at: www.statnews.com/2016/09/08/kratom-ban-hinders-research/. Accessed September 28, 2016.
- Halper E. DEA Ends Its Monopoly on Marijuana Growing for Medical Research. Los Angeles Times. August 11, 2016. Available at: www.latimes.com/politics/la-na-marijuana-dea-20160811-snap-story.html. Accessed September 28, 2016.
- Kratom (Mitragyna speciosa Korth). Drug Enforcement Administration website. Available at: www.deadiversion.usdoj.gov/drug_chem_info/kratom.pdf. Accessed September 28, 2016.
- Horie S, Koyama F, Takayama H, et al. Indole alkaloids of a Thai medicinal herb, Mitragyna speciosa, that has opioid agonistic effect in guinea pig ileum. Planta Medica. 2005;71(3):231-236. doi: 10.1055/s-2005-837822.
- Takayama H. Chemistry and pharmacology of analgesic indole alkaloids from the Rubiaceous plant, Mitragyna speciosa. Chem Pharm Bull. 2004;52(8):916-928.
- Manda VK, Avula B, Ali Z, Khan IA, Walker LA, Khan SI. Evaluation of in vitro absorption, distribution, metabolism, and excretion (ADME) properties of mitragynine, 7-hydroxymitragynine, and mitraphylline. Planta Medica. 2014;80(7):568-576. doi: 10.1055/s-0034-1368444.
- Ballabh P, Braun A, Nedergaard M. The blood-brain barrier: an overview: structure, regulation, and clinical implications. Neurobiol Dis. 2004;16(1):1-13.
- Chavkin C. The therapeutic potential of κ-opioids for treatment of pain and addiction. Neuropsychopharmacology. 2011;36:369-370. doi:10.1038/npp.2010.137.
- Pradhan AA, Befort K, Nozaki C, Gaveriaux-Ruff C, Kieffer BL. The delta opioid receptor: an evolving target for the treatment of brain disorders. Trends Pharmacol Sci. 2011;32(10):581-590. doi: 10.1016/j.tips.2011.06.008.
- Matsumoto K, Yamamoto LT, Watanabe K, et al. Inhibitory effect of mitragynine, an analgesic alkaloid from Thai herbal medicine, on neurogenic contraction of the vas deferens. Life Sciences. 2005;78(2):187-194.
- Tanguay P. Kratom in Thailand: Decriminalization and Community Control? Transnational Institute website. Available at: www.tni.org/files/download/kratom-briefing-dlr13.pdf. Accessed October 3, 2016.
- Agosti D. What is a treatment? Biosyscontext website. Available at: http://biosyscontext.blogspot.com/2011/02/what-is-treatment-on-way-to-define-or.html. Accessed October 6, 2016.
|