Issue:
127
Page: 36-45
Cannabidiol: A Race to Relief
by Nishi Whiteley, Ethan Russo, MD
HerbalGram.
2020; American Botanical Council Click here for PDF Click here for PDF
Few chemical compounds have enjoyed such a rapid ascent to market acceptance and consumer popularity as CBD. According to BDS Analytics, the US hemp-derived CBD market is projected to grow to $20 billion by 2024.1 CBD was the top-selling herbal dietary supplement in US natural retail stores in 2019, according to the American Botanical Council’s Herb Market Report. Sales in this retail channel grew 71.3% from 2018 to 2019, with total annual sales of $90.7 million in 2019.2 To hear the ever-increasing number of people who use the product extol its virtues, one might think it a cure-all. While that is not true, CBD is a versatile therapeutic compound that is well tolerated by many people, with few reports of serious adverse effects. Among its many potential benefits, CBD is a potent analgesic, antibiotic, anticonvulsant, anti-inflammatory, antipsychotic, and neuroprotective agent.3 It also has shown promising results in inhibiting tumor promotion in laboratory and animal studies.4 CBD deserves serious consideration not only as a medicine but also as an important component of health and wellness regimens.
CBD is known to be found only in the plant Cannabis sativa (Cannabaceae).5* The first known mention of cannabis in recorded text appeared around 2350 BCE in the Pyramid Texts from the Egyptian Old Kingdom in the ancient city of Memphis.6 In the thousands of years that humans have used cannabis as medicine, an intoxicant, and for spiritual purposes, no known deaths have been attributed to its use based on direct toxicological effects. 
CBD is one of more than 150 chemicals known as cannabinoids found to date in C. sativa. Although less is known about cannabinoid acids, the non-psychotropic chemical precursors of cannabinoids, they are also considered therapeutic and have shown promise as non-intoxicating medicines. In a 2013 study, cannabidiolic acid (CBDA) was found to be 1,000 times more potent than CBD in a rat model for the treatment of nausea and vomiting.7,8 Cannabinoid acids are decarboxylated (a process in which the carboxyl group in the cannabinoid acid molecule is removed) through heat, light exposure, or time, which converts the acid to a neutral cannabinoid. Tetrahydrocannabinolic acid (THCA) — a precursor of tetrahydrocannabinol (THC), the primary psychoactive and intoxicating compound in cannabis — and CBDA concentrations are 20-50 times higher than neutral cannabinoids in fresh dried plant material.3
Isolated by American chemist Roger Adams, PhD, in 1940, with the complete structure elucidated by Israeli chemist Raphael Mechoulam, PhD, in 1963, CBD is the second-most researched cannabinoid and the most abundant cannabinoid in hemp varieties of the cannabis plant. Unlike its counterpart THC, CBD does not make one feel psychologically altered or “high,” yet it crosses the blood-brain barrier when inhaled, producing anti-anxiety and antipsychotic effects, technically making it psychoactive.4 A high density of cannabinoid receptors exists in the human brain, but, unlike mu-opioid receptors, they are sparsely distributed in the parts of the brain stem that control heartbeat and breathing. 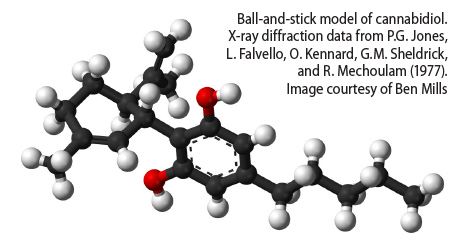
In June 2018, the US Food and Drug Administration (FDA) approved the first and only cannabis-derived CBD drug, Epidiolex® (GW Pharmaceuticals; Cambridge, UK), which was designated a Schedule V orphan drug (orphan drugs are designated for conditions affecting fewer than 250,000 people in the US). Epidiolex is approved for the treatment of seizures associated with Lennox-Gastaut and Dravet syndromes, both rare childhood forms of epilepsy, and tuberous sclerosis. In the same year, the US Farm Bill legalized hemp production and the production of hemp-derived CBD products in states that vote to allow them.9
Hemp is arbitrarily, but legally, defined by US law as cannabis with less than 0.3% THC (0.2% in Europe).9,10 As long as finished consumer products that contain CBD do not have more THC than these specified limits, they are considered legal in many jurisdictions of the world. This legal distinction has led to a largely unregulated market that is akin to the Wild West or a market free-for-all without production, labeling, and testing standards. The FDA continues to assess how to regulate CBD in food and dietary supplements.
The public’s fascination with and sharply increased demand for CBD have sparked a global race to identify and breed varieties of cannabis without or low in THC and rich in other active cannabinoids and terpenes.† Due to the longstanding federally illegal status of cannabis in the United States and much of the world, CBD was largely bred out of cannabis because the market was driven by recreational users in search of THC-rich cannabis. Now that it is apparent that CBD has great medical utility, significant resources have been poured into pharmacodynamic and pharmacokinetic research, product development, and production of CBD-rich cannabis (generally defined by industry as dried cannabis with at least 4% CBD). Such varieties are becoming easier to find given increasing demand. However, access to CBD-rich material that meets Good Agricultural Practice (GAP) and Good Manufacturing Practice (GMP) quality standards remains difficult.
It is important to mention that C. sativa is a bio-remediator. Whatever is in the soil — good or bad (e.g., agricultural chemicals, heavy metals, minerals, etc.) — will also be absorbed into various parts of the C. sativa plant, including the flowers where the cannabinoid acids and terpenes are produced.11 Thus, the authors believe it advisable to use CBD sourced from companies using organic production practices that meet GAP and GMP standards.
CBD products are available in varying forms of purity. CBD isolate, commonly referred to as “pure CBD,” should be free from all other phytocompounds and comes in powder form. “Broad spectrum” or “full spectrum” CBD oil includes other therapeutically active chemicals from the cannabis plant, such as cannabinoids, terpenes, and/or flavonoids.
Mechanisms of Action
In the 1990s, it was discovered that the human body produces endocannabinoids: endogenous compounds that mimic the pharmacology of phytocannabinoids, a class of chemicals derived from the cannabis plant and rarely found in other species. Endocannabinoids, along with cannabinoid receptors and a series of enzymes, make up the endocannabinoid system (ECS). This system regulates, modulates, and/or plays a major role in almost every biological function of the human body, including immunity, cognition, inflammation, nausea/vomiting, temperature regulation, and neuroprotection.12
Simply, the ECS is a homeostatic regulatory system that plays a role in helping humans to eat, sleep, protect, forget, and relax.13 The discovery of the ECS is one of the most important medical discoveries of our time. Understanding how it works and integrates with different body systems is paramount to understanding the origin of a large number of diseases and proactively managing the aging process.
Although CBD’s mechanisms of action have not yet been fully elucidated, more than 65 different targets were identified by 2015.14 CBD works within and apart from the ECS through numerous enzymes, ion channels, receptors, and transporters.13 CBD is a negative allosteric modulator (NAM) of the cannabinoid receptor type 1 (CB1; in other words, when CBD binds to a non-primary CB1 receptor site, it reduces the ability of THC to bind to the primary site), which partly explains why CBD has attenuating activity on THC-associated adverse events such as anxiety and tachycardia (fast heart rate), and may also contribute to its antipsychotic, antiseizure, and antidepressant effects.14,15 Evidence of this is seen in the clinical trials conducted for the whole-plant cannabis pharmaceutical preparation Sativex® (GW Pharmaceuticals), approved in 30 countries, not including the United States, for spasticity and cancer pain. The current recommended upper limit Sativex dose contains 32.4 mg of THC and 30 mg of CBD.
Low-dose stimulation of CB1 receptors has been shown to reduce anxiety and impart a calming effect by managing neurotransmitter release such that excessive neuronal activity is prevented. CB1 receptors also play a major role in reducing pain and inflammation and regulate cognitive function, sensory perception, movement, and posture control.16 CBD indirectly activates this receptor by delaying the enzymatic breakdown of the CB1 agonists anandamide and 2-arachidonoylglycerol (2-AG),17 thus allowing these endocannabinoids to stay in the body long enough to be therapeutic.16 This is how CBD increases endocannabinoid tone. (Endocannabinoid tone is a function of the numbers of receptors, whether they are active or inactive, the concentration of endocannabinoids, and the activity of their metabolic and catabolic enzymes.) CB1 receptors also are found in bone, reproductive, cardiovascular, adipose, and liver tissues.18
CBD, a potent anti-inflammatory agent, augments and stimulates the activity of the cannabinoid receptor type 2 (CB2),19 where it helps reduce pain and inflammation by mediating cytokine release from immune cells.20 Largely found in immune tissue but also throughout the peripheral nervous system, CB2 receptors regulate a wide range of physiological processes, including pain perception, inflammation, immune function, bone growth, neuroprotection, and stress response.18
In addition to interacting with CB1 and CB2, CBD also binds to a variety of other receptors and activates ion channels and transcription factors (Table 1).
Synergistic Effects
Almost 600 phytocompounds have been identified in cannabis, many of which synergize with CBD.21 The cannabinoids, terpenes, flavonoids, and other phytochemicals present in cannabis activate different therapeutic pathways in the body, complicating research and drug development in this area.
The way chemicals from the cannabis plant synergistically work together to potentiate and antagonize different actions/reactions in the body is called the “entourage effect,” a term coined by Israeli researchers Shimon Ben-Shabat, PhD, and Mechoulam.24 For example, CBDA increases the bioavailability of CBD by a factor of two.21 CBD is, among other things, anxiolytic,25 as are a variety of terpenes in cannabis, such as linalool, eucalyptol, trans-nerolidol (which also increases bioavailability of cannabinoids), and guaiol.21,26 Limonene, a terpene in cannabis and the primary component of lemon oil, is also anxiolytic, most likely through multiple mechanisms of action, including modulation of 5-HT1A receptors27; it is also pro-apoptotic in breast cancer cells28 and is highly synergistic with CBD.29 A cannabis therapeutic product including CBD, CBDA, and limonene would likely be effective against anxiety, working through multiple chemical pathways simultaneously to bring the body back into balance. Whereas CBD may be an effective compound for managing anxiety, having the optimal combinations of cannabinoids, terpenes, and other phytochemicals can contribute greatly to the increased efficacy of a preparation.
Mono- and sesquiterpenes give many plants their smell and contribute greatly to the effects felt when consuming cannabis and cannabis products. Approximately 200 terpenes have been found in the cannabis plant, representing 3-10% of the liquid (by weight) in the trichome, the gland protruding from the plant where the main therapeutic compounds like cannabinoids/mono- and sesquiterpenes are produced and retained.21 Approximately 50 terpenes regularly occur in North American-grown cannabis, 17 of which are most common.6 Most of the terpenes found in the cannabis plant are listed on the US “GRAS List” (referring to ingredients that are “generally recognized as safe” for use in food; see https://femaflavor.org).21,30
Terpenes are thought to contribute greatly to the entourage effect of cannabis, providing synergy and increased efficacy for the treatment of addiction, anxiety, bacterial and fungal infections, depression, epilepsy, inflammation, and pain.29 Terpenes are therapeutic in their own right and supported by in vitro and in vivo research showing strong antidepressant, antidiabetic, anticonvulsant, antibiotic, anti-allergenic, cytotoxic, antitumor, and anti-inflammatory effects.21 Like cannabinoids, terpenes activate different pathways in the body simultaneously to synergize with various cannabinoids and flavonoids, creating a complicated yet elegant chemical ballet. The review articles by Russo (2011) and Russo and Marcu (2017) are the most comprehensive articles on this subject to date.29,31
Of the 6,000 known flavonoids, 26 have been described in cannabis, including apigenin-7-O-β-D-glucuronide, cannflavin A, and luteolin-7-O-β-D-glucuronide.21,32 Little is known about how flavonoids contribute to the entourage effect; however, protective effects against inflammation have been shown in laboratory experiments.33 Many of the flavonoids found in cannabis contribute to the chemical ballet, further extending potential therapeutic effects of CBD in the body.
Much of the existing research has been carried out with single-molecule CBD, not with whole-plant materials with a full spectrum of cannabinoids, terpenes, and flavonoids present in the essential oil of CBD-rich cannabis. In many cases, when whole-plant preparations have been used, individual phytochemicals were not quantified or investigated to assess how they may have contributed to research outcomes. It is believed that whole-plant cannabis formulations are superior therapeutic agents compared to isolated molecules.29 For example, in general, THC and CBD in combination are more therapeutic than either would be on their own.34 Furthermore, a naturalistic study with 134 humans using smoked cannabis showed that cannabis varieties with more than 4% CBD attenuated short-term memory loss caused by THC.35 The impact of one particular chemical on another may be subtle but powerful, contributing greatly to the therapeutic benefit of the formulation.36
Therapeutic Benefits
CBD has significant therapeutic potential, especially for symptoms such as inflammation, sleep, anxiety, and pain that are commonly addressed with dietary supplements, nutraceuticals, and over-the-counter products. Clinical Trials
An appropriate place to begin is to review what has been learned from clinical trials on the single-molecule CBD product Epidiolex, an antiseizure medication. Even though Epidolex trials have not yet assessed the drug’s effects on inflammation, sleep, anxiety, and pain (see next section) — the most common reasons people try CBD — they provide a baseline for safety, tolerability, and drug interactions and show that CBD is a powerful antiseizure agent.
According to GW Pharmaceuticals’ website, a Phase III clinical trial on Epidiolex for the treatment of Lennox-Gastaut syndrome with 225 patients aged 2-55 years old showed similar results to previously conducted Phase III clinical trials. Patients took 20 mg/kg/day, 10 mg/kg/day, or placebo along with their current medications. The 20-mg group showed a median monthly reduction in seizures of 42%, compared to a 37% reduction in the 10-mg group and a 17% reduction in the placebo group. One patient dropped out in both the 10-mg group and the placebo group, and six patients dropped out of the 20-mg group. Although adverse events were recorded in the study, most were deemed to be mild to moderate, with 99% of trial participants choosing to continue to participate in an open-label extension of the trial.37
In a double-blind, placebo-controlled trial with 120 children and young adults with Dravet syndrome with drug-resistant seizures, seizure frequency decreased from a median of 12.4 to 5.9 seizures per month in the 20 mg/kg/day dose Epidiolex group compared to a decrease from a median of 14.9 to 14.1 seizures per month in the placebo group during the 14-week treatment period. Seizure activity was reduced in all types of seizures; 5% of the Epidolex group and 0% of the placebo group were seizure-free during the study. All patients in the study remained on their normal anti-epileptic drugs (AEDs).38
Pain and Inflammation
Cannabinoids have long been known as potent anti-inflammatory agents. According to a review by Nichols and Kaplan, CDB has been shown to produce these effects in rodent models:
- reduce immune response;
- prevent and reduce colitis;
- reduce β-amyloid-induced neuroinflammation;
- reduce interleukin 1 beta (IL-1β);
- decrease prostaglandin E2 (PGE2) plasma levels;
- enhance interferon gamma (IFN-γ) and IL-2 production;
- reduce tumor necrosis factor-alpha (TNF-α) level in frontal cortex;
- decrease hepatic reperfusion injury;
- reduce lipopolysaccharide (LPS)-induced pulmonary inflammation;
- reduce effects of autoimmune encephalomyelitis; and
- reduce inflammation in acute lung injury.22
In humans, CBD has been shown to inhibit neutrophil chemotaxis (migration of neutrophils to sites of infection)39 and reduce seizure severity, frequency, and recovery time.40
A 2010 multicenter, double-blind, randomized, placebo-controlled, parallel-group study with 177 subjects compared a 1:1 THC:CBD extract and a THC-only extract to placebo for efficacy, safety, and tolerability in patients with intractable cancer-related pain. The study results showed that the 1:1 THC:CBD extract improved pain scores by 30% from baseline in more than half of that group, whereas the THC-only group had no significant improvements over the placebo group. The preparations were administered in self-titrated oral mucosal sprays with 2.7 mg of THC and 2.5 mg of CBD per spray. Patients averaged 8.75 sprays per day in the THC:CBD group, 8.34 sprays per day in the THC-only group, and 9.61 sprays per day in the placebo group. While all three groups of study participants had similar baseline pain scores, only patients in the THC:CBD group showed a statistically relevant improvement in reduction of pain scores of 30% or more (23 subjects [43%] in the THC:CBD group, 12 subjects [23%] in the THC-only group, and 12 subjects [21%] in the placebo group).41
Pain and inflammation are inextricably linked. CBD has been shown in many mouse models to reduce inflammation and pain by indirectly suppressing the inflammatory response at the adenosine A2 receptor, binding to a variety of receptors, possibly including antagonism of GPR55 and modulating endocannabinoid tone at the TRPV1 and other TRP receptors. Furthermore, it appears that CBD may effectively potentiate the analgesic effects of opioids without aggravating constipation or depressing respiratory drive, thus modulating the risks of opioid addiction and side effects.15
CBD is a more potent neuroprotective antioxidant than tocopherols or ascorbate as demonstrated in rat neuronal cultures with respect to glutamate-induced neurotoxicity.42 In fact, the US government holds a patent (US patent 663050743) on cannabinoids for their antioxidant and neuroprotective effects.29 Interestingly, in a rodent model of Alzheimer’s disease, CBD and anandamide promoted neurogenesis after β-amyloid exposure.40 CBD also has been shown to prevent reactive oxygen species (ROS)-associated cell death and mediate glutamate-induced neurotoxicity.44 If confirmed in human clinical studies, the neuroprotective benefits of CBD stand to potentially improve quality of life for patients with a wide variety of neurological conditions including Alzheimer’s disease, Parkinson’s disease, Huntington’s disease, Tourette syndrome, traumatic brain injury, stroke, and more.
Sleep
Babson et al reviewed sleep research on cannabinoids in 2017 and found mixed and dose-dependent effects of CBD, with low doses being stimulating and high doses being sedating. In the case of Parkinson’s disease, Babson et al reported that CBD may reduce REM sleep behavior disorder.45 A balanced preparation of THC and CBD improves sleep for those with pain associated with many conditions, including rheumatoid arthritis, peripheral neuropathic pain, multiple sclerosis (MS), and intractable cancer pain. This has been demonstrated in Sativex (2.7 mg THC and 2.5 mg CBD per oromucosal spray) clinical trials for the treatment of muscle spasms and spasticity in patients with MS. More than 1,000 people are engaged in these long-term studies.46 Pure CBD is slightly stimulating in low to moderate doses, which the authors consider to be less than 200 mg. However, as seen in the Sativex trials, it appears that CBD and THC work synergistically to reduce sleep disturbances and improve sleep quality in doses ranging from as low as 2.5 mg each of THC and CBD and up to 15 mg each of THC and CBD before bed.
CBD is thought to play a role in sleep quality because of its anxiolytic effects.47 In a retrospective case series at a psychiatric clinic involving 72 adults suffering from a lack of sleep (n = 25) or anxiety (n = 47), 79.2% of patients (57) reported decreased anxiety and 66.7% of patients (48) had improved sleep scores during the first month, but the effects fluctuated throughout the study. Most patients received 25 mg CBD per day in a capsule, although a small number received higher dosages (50 mg or 75 mg per day). In all but three patients, CBD was well tolerated.47
Anxiety
Anxiety, according to the Anxiety and Depression Association of America, is the most common mental illness and affects 40 million adults in the United States annually. Skelley et al conducted a review of 233 journal articles about CBD and its impact on anxiety. Only six small randomized clinical trials (RCTs) and two case studies met their criteria for inclusion in their review, which found CBD does improve the clinical outcomes for chronic and acute anxiety.48 Studies by Zuardi et al (2017)49 and Linares et al (2019)50 included multiple dose ranges for acute anxiety, with the best clinical outcomes at their mid-range dose of 300 mg. On the topic of social anxiety disorder, Bergamaschi et al (2011)51 conducted one of the earliest small trials. In addition to reduced acute anxiety and fewer interruptions in cognition, they found that “negative self-evaluation was almost abolished” in the CBD group versus the placebo group. More investigation is needed to better understand optimal starting doses for treating acute versus chronic anxiety.
In a yet-to-be-published CBD clinical trial in humans with chronic anxiety, 10 mg of a full-spectrum CBD oil (made from whole-plant cannabis containing additional unknown potentially synergistic phytochemicals such as minute amounts of other cannabinoids, terpenes, and flavonoids) given three times per day over four weeks resulted in less severe anxiety, fewer symptoms related to anxiety, and improved sleep and quality of life compared to baseline.52 CBD was well tolerated. Improved performance was noted in measures of executive and cognitive function such as memory, attention, and decision making. Given that recreational cannabis use has acutely been associated with decrements in executive functioning, this is significant. Small decrements were observed in verbal learning while verbal memory remained intact.
Drug Interactions
Low to moderate doses of CBD rarely cause drug interaction problems. However, relevant interactions have been documented at higher doses. Clobazam, an antiseizure drug, is metabolized by cytochrome P450, as is CBD and a wide variety of other drugs. When these kinds of drugs are used together with high doses of CBD, patients can experience unwanted side effects, the most common of which include drowsiness, irritability, and ataxia (impaired balance or coordination).53 Drug-drug interactions have also been observed with valproic acid with either higher or lower serum levels encountered.
Misconceptions
One of the biggest misconceptions regarding CBD is that it is sedating. On the contrary, low-to-moderate doses are highly alerting, and stimulating effects have been seen in studies in which patients received a single dose of a CBD isolate (CBD only) as high as 600 mg.3 Low-to-moderate dose CBD-related sedation can generally be attributed to the presence of the terpene myrcene in the preparation.29
Another common misconception is that CBD turns into THC when exposed to gastric acids via oral consumption. A study published in 2016 gave credence to this myth by reporting that CBD is converted to THC with prolonged exposure to simulated gastric fluids without enzymes.54 However, there is no evidence that this occurs in humans.3 To this point, multiple CBD studies, including studies in which large doses were given, failed to reveal a conversion to THC or the primary hepatic metabolite of THC, 11-hydroxy-THC.55 Brazilian researchers recently studied the blood of 60 men and 60 women after oral intake of 300 mg CBD and confirmed prior results of no bioconversion from CBD to THC.56
It often is assumed that CBD does not cause adverse events. This is not true. However, side effects of CBD generally are considered mild and cease by adjusting the dose or stopping consumption. The most commonly reported side effects of Epidiolex include somnolence (drowsiness), sleep disruption, diarrhea, fatigue, lethargy, and decreased appetite, but all of these adverse events are usually associated with high doses and frequently in association with polypharmacy.
Conclusion
While we are a long way from understanding all of the intricacies of cannabis therapeutics, we do know that at low-to-moderate doses, CBD is a safe, efficacious product with minimal adverse side effects, low toxicity, and fairly low risk for dangerous drug interactions. The promise of properly constituted CBD preparations for improving public health is great for treatment and prevention of a wide variety of diseases, conditions, and ailments. While over-the-counter market acceptance of CBD has occurred at rapid rates, clinical research has not advanced as quickly. Luckily, attitudes and laws are changing worldwide in a way that may positively impact research in this area.
Nishi Whiteley is the chief operating officer and co-founder of CReDO Science, a biopharmaceutical holding company dedicated to commercializing patented products generated from CReDO’s investigation of the cannabis plant and the endocannabinoid system. Whiteley has 30 years of business development experience and 10 years as a cannabis researcher, writer, educator, and advocate. She was a contributing science author at ProjectCBD.org, a member of the executive team at the International Cannabis and Cannabinoids Institute, and is the curator of the educational website MyChronicRelief.com. Whiteley is the author of the 2016 book Chronic Relief: A Guide to Cannabis for the Terminally & Chronically Ill (Alivio, LLC).
Ethan Russo, MD, is a board-certified neurologist, psychopharmacology researcher, and the founder and CEO of CReDO Science. Previously, he was the director of research and development for the International Cannabis and Cannabinoids Institute (2017-2019), medical director of PHYTECS (2015-2017), and, from 2003-2014, senior medical advisor, medical monitor, and study physician at GW Pharmaceuticals for numerous Phase I-III clinical trials of Sativex and Epidiolex. He was a clinical neurologist in Missoula, Montana, for 20 years. He has held faculty appointments in pharmaceutical sciences at the University of Montana and in medicine at the University of Washington. He is author/editor of seven books and has published more than 50 peer-reviewed articles.
References
- The Global Cannabinoids Market: Will CBD Overtake THC? [white paper] Boulder, CO: BDS Analytics; 2019.
- Smith T, May G, Eckl V, Morton Reynolds C. US Sales of Herbal Supplements Increase by 8.6% in 2019. HerbalGram. 2020;127:54-67.
- Russo EB. Cannabidiol claims and misconceptions. Trends Pharmacol Sci. 2017;38:198-201. doi: 10.1016/j.tips.2016.12.004.
- Ladin DA, Soliman E, Griffin L, Van Dross R. Preclinical and clinical assessment of cannabinoids as anti-cancer agents. Front Pharmacol. 2016;7:361. Available at: www.frontiersin.org/articles/10.3389/fphar.2016.00361/full. Accessed January 10, 2020.
- Piomelli D, Russo EB. The Cannabis sativa versus Cannabis indica debate: An interview with Ethan Russo, MD. Cannabis Cannabinoid Res. 2016;1(1):44-46. Available at: www.ncbi.nlm.nih.gov/pmc/articles/PMC5576603/. Accessed July 29, 2020.
- Russo E. History of Cannabis and its preparations in saga, science & sobriquet. Chemistry & Biodiversity. August 2007;4(8):1614-1648.
- Bolognini D, Rock E, Cluny N, et al. Cannabidiolic acid prevents vomiting in Suncus murinus and nausea-induced behavior in rats by enhancing 5-HT1A receptor activation. Br J Pharmacol. 2013;168:1456–1470.
- Rock EM, Parker LA. Effect of low doses of cannabidiolic acid and ondansetron on LiCl-induced conditioned gaping (a model of nausea-induced behaviour) in rats. Br J Pharmacol. 2013;169(3):685-692. doi: 10.1111/bph.12162.
- H.R. 2 - The Agriculture Improvement Act of 2018 (P.L. 115-334). 115th Congress (2017-2018).
- European Monitoring Centre for Drugs and Drug Addiction. Cannabis Legislation in Europe: An Overview. Luxembourg: Publications Office of the European Union; 2017.
- Husain R, Weeden H, Bogush D, et al. Enhanced tolerance of industrial hemp (Cannabis sativa L.) plants on abandoned mine land soil leads to overexpression of cannabinoids. PLoS One. 2019;14(8):e0221570. Available at: www.ncbi.nlm.nih.gov/pmc/articles/PMC6715179. Accessed June 21, 2020.
- Petrocellis LD, Cascio MG, Di Marzo V. The endocannabinoid system: A general view and latest additions. Br J Pharmacol. 2004;141:765-774. doi:10.1038/sj.bjp.0705666.
- Di Marzo V, Melck D, Bisogno T, De Petrocellis L. Endocannabinoids: Endogenous cannabinoid receptor ligands with neuromodulatory action. Trends Neurosci. 1998;21:521-528.
- Laprairie RB, Bagher AM, Kelly ME, Denovan-Wright EM. Cannabidiol is a negative allosteric modulator of the type 1 cannabinoid receptor. Br J Pharmacol. 2015;172:4790-4805.
- Bih CI, Chen T, Nunn AVM, Bazelot M, Dallas M, Whalley BJ. Molecular targets of cannabidiol in neurological disorders. Neurotherapeutics. 2015;12:699-730.
- Leweke FM, Piomelli D, Pahlisch F, et al. Cannabidiol enhances anandamide signaling and alleviates psychotic symptoms of schizophrenia. Transl Psychiatry. 2012;2:e94. doi: 10.1038/tp.2012.15.
- Bisogno T, MacCarrone M, De Petrocellis L, et al. The uptake by cells of 2-arachidonoylglycerol, an endogenous agonist of cannabinoid receptors. Eur J Biochem. April 2001;268(7):1982-9. doi: 10.1046/j.1432-1327.2001.02072.x. Available at: https://pubmed.ncbi.nlm.nih.gov/11277920/. Accessed June 21, 2020.
- Whiteley N. Chronic Relief: A Guide to Cannabis for the Terminally and Chronically Ill. Austin, Texas: Alivio LLC; 2016.
- Martinez-Pinilla E, Varani K, Reyes-Resina I, et al. Binding and signaling studies disclose a potential allosteric site for cannabidiol in cannabinoid CB2 receptors. Front Pharmacol. 2017;8:744.
- Mechanism of action. GW Pharmaceuticals website. Available at: www.gwpharm.com/healthcare-professionals/research/mechanism-action/. Accessed March 3, 2020.
- Nehler G, Jones TM, Russo EB. Cannabidiol and contributions of major hemp phytocompounds to the “entourage effect”; possible mechanisms. J Alterative, Complementary & Integr Med. 2019;5:70.
- Nichols J, Kaplan BLF. Immune responses regulated by cannabidiol. Cannabis and Cannabinoid Research. 2020;5(1):12-31. doi:10.1089/can.2018.0073.
- Russo E, Guy GW. A tale of two cannabinoids: The therapeutic rationale for combining tetrahydrocannabinoil and cannabidiol, Medical Hypothesis. February 2006.
- Ben-Shabat S, Fride E, Sheshkin T. An entourage effect: inactive endogenous fatty acid glycerolesters enhance 2-arachadonol-glycerol cannabinoid activity. European Journal of Pharmacology. 1998;353:23-31.
- Zuardi AW, Cosme RA, Graeff FG, Guimarães FS. Effects of ipsapirone and cannabidiol on human experimental anxiety. J Psycho Pharmacol (Oxford). 1993;7(1)(Suppl.):82-88.
- Ceremuga TE, McClellan CB, Green XC, et al. Investigation of the anxiolytic and antidepressant effects of eucalyptol (1,8-cineole), a compound from eucalyptus, in the adult male Sprague-Dawley rat. AANA Journal. 2017:85(4):277-284.
- Komiya M, Takeuchi T, Harada E. Lemon oil vapor causes an anti-stress effect via modulating the 5-HT and DA activities in mice. Behav Brain Res. 2006;172:240-249.
- Vigushin DM, Poon GK, Boddy A, et al. Phase I and pharmacokinetic study of d-limonene in patients with advanced cancer. Cancer research campaign phase I/II clinical trials committee. Cancer Chemother Pharmacol. 1998;42(2):111-117.
- Russo E. Taming THC: Potential cannabis synergy and phytocannabinoids-terpenoid entourage effects, Brit J of Pharma. 2011;163:1344-1364.
- FEMA GRAS. Flavor and Extract Manufacturers Association of the United States website. Available at: www.femaflavor.org/fema-gras. Accessed March 3, 2020.
- Russo EB, Marcu J. Cannabis pharmacology: The usual suspects and a few promising leads. Advances in Pharmacology. 2017;80:67-134.
- Pollastro F, Minassi A, Fresu LG. Cannabis phenolics and their bioactivities. Current Medicinal Chemistry. 2017;24(10):1-42.
- Alam MN, Almoyad M, Huq F. Polyphenols in colorectal cancer: Current state of knowledge including clinical trials and molecular mechanism of action. Biomed Res Int. 2018;2018:4154185.
- McPartland J, Russo E. Cannabis and Cannabis extracts: Greater than the sum of their parts? J Cannabis Therapeutics. 2011;3(104).
- Morgan C, Shafer G, Freeman TP, Curran V. Impact of cannabidiol on the acute memory and psychomomitec effects of smoked cannabis: A naturalistic study. British Journal of Psychiatry. 2010;197(4):285-290.
- Corroon J, Feliece JF. The endocannabinoid system and its modulation by cannabidol (CBD). Alternative Therapies. 2015 Oct;12(4):692–698.
- GW Pharmaceuticals Announces Positive Phase 3 Pivotal Trial Results for Epidiolex® (cannabidiol) in the Treatment of Lennox-Gastaut Syndrome. [press release] London, UK: GW Pharmaceuticals; June 27, 2016.
- Devinsky O, Cross JH, Laux L, et al. Cannabidiol in Dravet syndrome study group. Trial of cannabidiol for drug-resistant seizures in the Dravet syndrome. N Engl J Med. May 2017;376:2011-2020.
- McHugh D, Tanner C, Mechoulam R, Pertwee RG, Ross RA. Inhibition of human neutrophil chemotaxis by endogenous cannabinoids and phytocannabinoids: Evidence for a site distinct from CB1 and CB2. Molecular Pharmacology. February 2008;73(2):441-450.
- Esposito G, Scuderi C, Valenza M, et al. Cannabidiol reduces Ab-induced neuroinflammation and promotes hippocampal neurogenesis through PPARg involvement. PLoS ONE. 2011;6(12):e28668. doi: 10.1371/journal.pone.0028668.
- Johnson JR, Burnell-Nugent M, Lossignol D, DoinaGanae-Motan E, Potts R. Multicenter, double-blind, randomized, placebo-controlled, parallel-group study of the efficacy, safety, and tolerability of THC:CBD extract and THC extract in patients with intractable cancer-related pain. J Pain & Symptom Mgmt. 2010;39(2):167-179.
- Russo E. Cannabis therapeutics and the future of neurology. Frontiers in Integ Neurosci. 2018;12:51.
- Hampson AJ, Julius A, Grimaldi M, inventors; The United States of America as represented by the Department of Health and Human Services, assignee. Cannabinoids as antioxidants and neuroprotectants. US patent 6,630,507. October 7, 2003.
- Hampson AJ, Grimaldi M, Axelrod J, Wink D. Cannabidiol and(−)∆9-tetrahydrocannabinol are neuroprotective antioxidants. Proc Natl Acad Sci USA. July 1998;95(14):8268 8273. doi: 10.1073/pnas.95.14.8268.
- Babson KA, Sottile J, Morabito D. Cannabis, cannabinoids, and sleep: Review of the literature. Current Psychiatry Report. April 2017;19:23.
- Russo E, Guy G, Robson P. Cannabis, pain, and sleep: Lessons from therapeutic clinical trials of Sativex®, a cannabis based medicine. Chemistry & Biodiversity. August 2007;4:1729-1743. doi:10.1002/cbdv.200790150.
- Shannon S, Lewis N, Lee H, Hughes S. Cannabidiol in anxiety and sleep: a large case series. Perm J. 2019;23:18-41. doi: 10.7812/TPP/18-041.
- Skelley J, Deas C, Curren Z, Ennis J. Use of cannabidiol in anxiety and anxiety-related disorders Journal of the American Pharmacists Association.
2019;60(1):253-261. https://dx.doi.org/10.1016/j.japh.2019.11.008.
- Zuardi AW, Rodrigues NP, Silva AL, et al. Inverted U-Shaped Dose-Response Curve of the Anxiolytic Effect of Cannabidiol during Public Speaking in Real Life. Front Pharmacol. 2017;8:259. doi: 10.3389/fphar.2017.00259.
- Linares IM, Zuardi AW, Pereira LC, et al. Cannabidiol presents an inverted U-shaped dose-response curve in a simulated public speaking test. Braz J Psychiatry. 2019;41:9-14. doi: 10.1590/1516-4446-2017-0015.
- Bergamaschi MM, Queiroz RH, Chagas MH, de Oliveira DC, De Martinis BS, Kapczinski F. Cannabidiol reduces the anxiety induced by simulated public speaking in treatment-naive social phobia patients. Neuropsychopharmacol. 2011;36(6):1219-1226. http://dx.doi.org/10.1038/npp.2011.6.
- Gruber S. A Little Piece of MIND: Examining Data from the First Longitudinal Study of Medical Cannabis. CanMed Conference Presentation. Pasadena, California. September 23, 2019.
- Geffrey AL, Pollack SF, Bruno PL, Thiele EA. Drug-drug interaction between clobazam and cannabidiol in children with refractory epilepsy. Epilepsia. 2015;56(8):1246-1251.
- Merrick J, Lane B, Sebree T, Yaksh T, O’Neill C, Banks SL. Identification of psychoactive degradants of cannabidiol in simulated gastric and physiological fluid. Cannabis Cannabinoid Res. 2016;1:102-112.
- Grotenhermen F, Russo E, Zuardi AW. Even high doses of oral cannabidiol do not cause THC-like effects in Humans: Comment on Merrick et al. Cannabis and Cannabinoid Research. Dec 2017. http://doi.org/10.1089/can.2016.0036.
- Crippa JAS, Zuardi AW, Hallak JAC, et al. Oral cannabidiol does not convert to ∆8-THC or ∆9-THC in humans: A pharmacokinetic study in healthy subjects. Cannabis and Cannabinoid Research. February 2020;5(1):89-98.
|