Issue: 22 Page: 19
Hawthorn: A LITERATURE REVIEW.
by Steven Foster, Christopher Hobbs
HerbalGram. 1994; 22:19 American Botanical Council
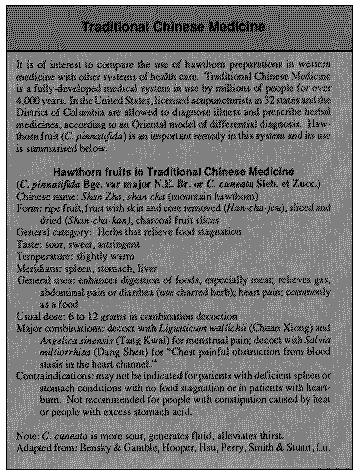
The hawthorn tree [Crataegus laevigata (Poiret) DC] is richly endowed with associations of May-time rituals from times before medieval England. The fruits (haws) were eaten as a food and made into wine throughout Europe since the Middle Ages. The ancient Greeks and Romans do not write of its virtues in medicine, but beginning in the Renaissance the fruits and leaves were considered good remedies for digestive and urinary tract ailments. In the late 1800s, European doctors began experimenting with it clinically for heart disease and other cardiovascular disorders and since then its reputation has grown steadily. Today many laboratory tests and a number of clinical trials support its use by demonstrating that hawthorn leaves, flowers, and fruits contain chemical compounds that increase blood flow to the heart muscle as well as positively affect other aspects of cardiovascular health. The following article reviews the botany, history of use, chemistry, pharmacology, toxicology, and pharmacy of hawthorn and its commercial preparations.In both the East and West, hawthorn has been used for millenia as both a food and a medicine. Today hawthorn preparations are used extensively in France, England, Germany, Russia, and other European countries, especially for the treatment of heart and cardiovascular ailments. BOTANY Taxonomy Crataegus is a genus of the Rosaceae (rose family), with approximately 280 species native to northern temperate zones primarily concentrated in East Asia, Europe and Eastern North America. Some species are found in central and southwestern Asia. The vast majority of the North American species occur in the eastern regions, from Newfoundland to mountains of northern Mexico (Sargent 1933). Hawthorn is a highly complex and technical plant group. W.H. Duncan and M.B. Duncan (1988) note that Crataegus is difficult to define in terms of numbers and species because of hybridization and unusual factors relative to reproduction, including 1) apomixis, or the development of an embryo from cells other than sex cells; 2) polyploidy, where chromosome numbers are increased by 1,2,3,4-fold or more; and 3) anauploidy, in which chromosome numbers are in multiples other than those involved in polyploidy. A number of species are valued for economic use as food, medicine, and ornamentals. Crataegus laevigata (Poir.) DC. (C. oxyacantha auct. non. L.) English Hawthorn, Haw, Whitethorn, or aubepine (French) is widely used as a source plant for Crataegus drugs. Crataegus laevigata is the C. oxyacantha of ancient Latin authors. The two are often confused. Crataegus oxyacantha L. is most commonly listed as the source plants for hawthorn preparations. Crataegus monogyra Jacq. also is used for production of hawthorn fruits. Crataegus pinnatifida Bge., C. pinnatifida var. major N.E. Br., and C. cuneata Sieb. et Zucc. are used as source plants for the Chinese drug Shan-zha (dried hawthorn fruit). These three taxa are official in the Pharmacopeia of the People's Republic of China (Mabberly 1988, Tucker et al. 1989, Lou 1987, Pharmacopeia Committee 1985). Crataegus laevigata occurs in much of northern Europe and has become naturalized in eastern North America and India. It was brought to North America by early European colonists as an ornamental, primarily as a hedge plant. American species were also introduced to Europe at an early date (Emerson 1875). The Chinese C. pinnatifida is also found in European and American horticulture. Crataegus pinnatifida var. major is distributed in north and northeast China, where most of the supply is cultivated. Crataegus pinnatifida is distributed in northeast China, north China, Shanxi and Jiangsu provinces. The former taxa are known as "Northern Hawthorn" fruits. Chief production provinces include Shangdong, Henan and Hebei. Crataegus cuneata, known as "Southern Hawthorn," is primarily distributed in the Changjian valley in Guangdong and Guangxi provinces. Major production areas include Zhejiang and Jiangsu provinces (Lou 1987). Description Crataegus species are much-branched shrubs or small spreading trees, usually (though not always) armed with long slender thorns. The deciduous leaves are simple, usually ovate to elliptical, pinnately veined, serrate, dentate, or with shallow-lobed margins. Leaves are larger and more lobed on young branchlets. Flowers are usually produced in spring on simple or branched terminal corymbs, sometimes singly or in clusters of twos or threes. The perfect, radially symmetrical flowers have 5 petals, often pink in bud, then turning white or pink in full bloom, and 5 sepals persistent following anthesis. The yellowish-green to yellow, orange, or, more commonly, red globular fruits, are a berrylike pome with 1-5 small one-seeded nutlets. The flesh is dry-firm to succulent. In one species, Blueberry Hawthorn, C. brachycantha Sarg. & Engelm., the fruits are bright blue and glaucous. (Godfrey 1988, Little 1980, Duncan and Duncan 1988.) Descriptions of the genus are relatively vague at best. According to Eggleston (1908), "The genus is so variable that it is impossible to find characters which will hold absolutely true, either between species or even sections; then again, characters which seem to hold good in one section are useless in the next." (Eggleston, 1908, p. 74.) NOMENCLATURE Dioscorides, the most reliable of the ancient authors on plant medicines, called Crataegus "Oxuakantha," which was retained by Linnaeus in the name C. oxyacantha, an old name for C. laevigata. Although many botanical and herbal writers from the 15th through the 17th centuries took Dioscorides' Oxuakantha to be a kind of Crataegus, Parkinson (1640) determined that it was likely a Pyracantha. It is listed as C. pyracantha in Gunther's edition of Dioscorides (1933). The Oxuakantha described by Dioscorides is now referred to as Pyracantha coccinea (Crataegus pyracantha) (Pickering 1879, L.H. Bailey Hortorium 1976). Pyracantha is a genus not particularly lauded for its healing properties. Galen's "Oxyacanthus" is also certainly a Pyracantha, Pyrus or Mespilus (medlar). The latter three genera are closely allied and until the 17th century were likely to be poorly distinguished from Crataegus (Parkinson). Theophrastus (Hort), the most important Greek writer on botany describes a type of hawthorn (C. laevigata according to Hort) as a kind of medlar (Mespilus) under the name "Anthedonoeides." Pliny (Jones), a great compiler who was not above plagiarising from other sources, said this of the plant: By crataegos or crataegon Theophrastus would have us understand the tree which in Italy is called aquifolium. Gerard (1633) called hawthorn oxyacanthus, white thorne, or hawthorn tree. The latter two, and the name "May-Bush," are still common in England. In Germany hawthorn is now called Weiádorn (White Thorn), while in France it is referred to as l'epine noble (the noble thorn) because it was supposedly used for Christ's crown of thorns. Crataegus species are also variously known as Hawthorn, Haw, Thornapple (Ed. note -- not to be confused with Datura), Red Haw, Hog-apple, and many other common names. Haw is derived from an ancient word referring to hedge. The generic name Crataegus, derived from the Greek Kratos, meaning strength, in reference to the hardness of the wood, is attributed to Theophrastus. The specific epithet, "oxyacantha," attributed to Disocorides, is a Greek name that has been applied by ancient writers to barberry, sweetbriar, hawthorn, and other plant groups. Oxy means sharp and acantha, a thorn (Alcock 1876). HISTORY OF USE The history of the medicinal use of hawthorn seems to be relatively short. As detailed above, it is doubtful if the ancients wrote about hawthorn. It is not mentioned in the late Latin works Herbarium Apuleii Platonici (1000-1050) or Macer Floridus (8491112), or the early Anglo-Saxon herbals (Cockayne), such as the Leechbook of Bald or Lacnunga from 900-1100 A.D. In the Arabian school, C. azarolus L., a Mediterranean hawthorn, is mentioned by Al-Samarqandi (ca. 1210 A.D.) as being "useful for the stomach and yellow gall" (Levey & Al-Khaledy). In the late 16th and early 17th centuries it was mentioned in Parkinson and Gerard. Gerard noted (1597) only that the fruits are very astringent, and quoted Dioscorides's discussion of Pyracantha coccinea, which does not concern hawthorn proper. Parkinson (1640) wrote about the ripe berries or the seeds being "a singular good remedy against the stone" (kidney stones), or taken in wine for dropsy, saying also that the flowers steeped in wine" is a soveraigne remedy for the plurisie." According to Sowerby, school children in late medieval England gathered hawthorn branches for the maypole which they danced around during the May festival in honor of Flora. This custom was preserved in Europe through the 1800s. The Romans also used hawthorn's hard wood for carving and making walking sticks. Over the centuries legends about hawthorn have abounded in England and Europe. The poets, too, have sung its praises, as in Chaucer's phrase: Marke the faire blooming of the Hawthorne tree Who finely cloathed in a robe of white, Fills full the wanton eye with May's delight. Goldsmith, in his "Deserted Village," penned these well-known lines: The Hawthorn-bush with seats beneath the shade, For talking age and whispering lovers made. It appears that the current use of hawthorn for heart conditions dates back to the 17th century, according to Leclerc (Madaus), though in 1733, Alleyne in his The New English Dispensatory writes only of its use as a diuretic and"powerful expeller(s) of the stone and gravel." He states further that the flowers were the main ingredient in the famous "nephritic water." Green, an Irish doctor, is known to have used it extensively for heart ailments and, after his death in 1894, it is said to have become a famous remedy for this purpose. In Europe, both homeopathic and allopathic doctors used the herb for various heart and cardiovascular ailments from the late 19th through the early 20th centuries -- and with great clinical success. Hawthorn had entered American clinical practice by 1896 (Madaus). Assmann (Madaus), a homeopathic doctor, said the following regarding hawthorn's use as a cardiac medicine: Crataegus is no panacea, but for the handling of chronic illness, it is much more suitable than digitalis and strophanthus, because it has no unpleasant side-effects and no cumulative effects. Its success can be achieved if the tincture of the fresh ripe fruit in a suitable dose (3 times daily 10-20 drops after meals) is prescribed. In North America, Crataegus species were first observed by the Jacques Cartier expedition to Canada of 1535-6. Many "thorns" were observed including hawthorns, which were compared to the European medlars. Subsequent English and French expeditions to the New World in the late sixteenth and early seventeenth centuries noted the presence of "medlars" larger than those in Europe (Erichsen Brown 1979). Rafinesque (1830) mentions Crataegus. He writes, "Fruits of several edible, red or yellowed, acid, or sweetish, making fine stomachic preserves, useful for diarrhea and antiemetic; such as Cr. coccinea, Cr. tomentosa, Cr. crusgalli. The leaves and flowers of this last, used as pectoral in coughs and whooping cough, as a tea..." (Rafinesque, 1830, p. 213.) In his ethnobotanies of the Meskwaki, Ojibwe, and Potawatomi, H.H. Smith mentioned a number of medicinal uses, including the use of the fruits for bladder ailments, the tea for pain in the side, and bladder troubles, general debility, and as a medicine for stomach complaints (Erichsen-Brown 1979). Except for passing references, hawthorns are largely absent from the materia medica of nineteenth century America, until the publication of an article by J.C. Jennings of Chicago in 1896. According to J.U. Lloyd (1917) this is the first conspicuous American reference to the use of Crataegus in the treatment of heart disease. Lloyd writes: "A well-known physician, the late Dr. Green, of Ennis, County Clare, Ireland, attained an extended reputation in the treatment of `Heart Disease,' keeping the remedy a secret. Upon his death, in 1894, his daughter revealed the fact that this `famous' cure was a tincture of the ripe berries of Crataegus Oxycanthus." (J.U. Lloyd 1917. p. 2.) Following the publication of Jennings's 1896 paper in the New York Medical Journal, a number of physicians engaged the services of Lloyd Brothers to introduce a preparation of the ripe fruits of hawthorn to the medical practice. They investigated numerous species of Crataegus and made several preparations, including tincture of European hawthorn berry and tinctures of the bark and root. Lloyd claims to have found that one American species was superior to that of the imported C. laevigata (C. oxycantha). Unfortunately Lloyd does not reveal the identity of the American species used in the Lloyd Brothers preparations. The species name is also not given on the Lloyd Brothers product label, which states: "Specific Indications and Uses: Functional and organic heart affections, with pain, dyspnea, precordial oppression, rapid and feeble heart-action; valvular insufficiency; cardiac hypertrophy; marked anemia; venous stasis; angina pectoris; endocarditis following inflammatory rheumatism." (Anon. 1927) A number of articles from the medical literature from 1896 1916, including case histories, are reproduced in the Lloyd Brothers Treatise on Crataegus (Lloyd 1917). While mentioned in early texts for use as a diuretic, astringent, or in the treatment of dyspepsia, historical references to the cardiac-affecting properties of hawthorn fruits are absent from the literature prior to 1896. In the first two decades of this century, numerous articles and case histories on the use of hawthorn in heart disease appeared in medical textbooks and the periodical literature, primarily of Eclectic physicians. Crataegus is barely mentioned in passing in official medical texts such as The United States Dispensatory and is absent in the United States Pharmacopeia. The fruits of three taxa are official in the Pharmacopeia of the People's Republic of China. The Chinese drug Shan-Zha is first mentioned in the Tang Ben Cao (659 A.D.), attributed to Su Jing and 23 other scholars. Published during the Tang dynasty (618-907 A.D.), it is considered the world's earliest officially published pharmacopeia (Hsu 1986, Hou 1977). In Chinese tradition the fruits are used to improve digestion, eliminate stagnated food, and blood stasis, in the treatment of dyspepsia, lack of milk secretion, fullness in the stomach, abdominal distention, menorrhalgia, postpartum abdominal pain due to blood stasis, and hyperlipemia (Lou 1987). CULINARY USES AND REGULATORY STATUS In medieval England, children ate the plant's fruit, which was considered to be very nutritious. The fruit was also used in Russia to make wine (Sowerby). In some regions of Europe the dry pulp of the fruits of C. laevigata and C. monogyna has been eaten or added to flour. In West Asia, the larger, more fleshy and flavorful fruits of C. aronia (L.) Bosc. (C. azarolus) are commonly harvested from the wild and eaten fresh. These two species are variable. In their native ranges, seed from superior forms is selected and planted at field edges or on non-arable land. The fruits are collected from the mountains around Peking and other parts of China and mixed with sugar to make a jam or jelly or a sweet wine. These, along with candied fruit slices, are commonly sold in markets and by street vendors. The sweet and sour flavor is thought to support and activate the digestion (Lu, Smith & Stuart, Hooper). The nutlets of C. laevigata and C. monogyna have been found at a number of archeological sites in Europe, from the Neolithic to Roman time. Crataegus aronia seeds have been found in Bronze Age sites in Israel, as well as other archeological sites in the Near East (Zohary and Hopf 1988). At least a dozen species of Crataegus are documented as food plants of various native groups of North America. Often the fruits were dried and stored for winter use. For an enumeration of native groups that used hawthorn as food, plus references, see E. Yanovsky (1936). English or May Hawthorn (C. oxyacantha L.) is listed in a now-outdated FDA Policy Guideline as an "herb of undefined safety." (FDA Internal Memo, Nov. 19, 1975.) Currently, hawthorn leaves and berries have no official regulatory status in the U.S. CHEMISTRY AND PHARMACOLOGY In the case of hawthorn, the discovery and characterisation of isolated constituents was closely associated with research on their pharmacological activities. For this reason, the chemistry and pharmacology sections are here combined. Early Work (1850-1960) The first chemical analyses of hawthorn were performed on the European species (C. laevigata, C. monogyna, and occasionally C. pentagyna), and focused on the fruits and flowers, which have been considered the most active parts since the middle of the 19 th century. Wicke isolated trimethylamines from the flowers of hawthorn as early as 1854, which Madaus reported and claimed to play a possible role in hawthorn's activity (Madaus). However, recent work on the cardioactive amines of C. laevigata shows that they quickly break down in the digestive tract and thus are probably inactive in oral preparations (Wagner & Grevel, 1982). As early as 1897, Madaus also reported on the peripheral vessel effects of quercitrin and quercetin, the latter being a common flavonoid discovered in hawthorn. In 1927, Baechler reported (Bersin & Müller) that the effective constituent of the fruits was crataegus acid, which was later found to be a mixture of triterpene carboxylic acids. Schimert asserted that these carboxylic acids were responsible for the coronary dilating effects of hawthorn (Nikolov, 1969), though several later investigations failed to support his claim (Nikolov, 1969; Sajner). The first compound that proved to be cardioactive in test animals was heptahydroxyflavane glycoside (Nikolov, 1969). It is noteworthy that most early and later work on hawthorn was conducted on animals, not humans. This is surprising considering that hawthorn has shown extremely low toxicity in every animal species tested. There is a need for more practical information about hawthorn's effects on the human cardiovascular system. The early experiments on Crataegus extracts used intravenous, intraperitoneal, or, rarely, subcutaneous injections of various flavonoid fractions (either water, methanolic, or ethanolic extracts) into the usual array of test animals -- dogs, frogs, mice, rats, guinea pigs, cats, etc. Only a few tests involved oral administration. The general results of these studies are shown in Table 1, summarized from Ammon and Händel (1981b,c). It should be noted, however, that the injection of alcohol (EtOH) itself can lead to vasodilation of the coronary arteries, increasing blood flow to the heart (Kanno, et al.). Thus, tests performed with ethanolic or methanolic extracts must be examined closely regarding any such effects. These data are, of course, more pertinent to clinical applications in Europe, where injectable preparations of Crataegus extracts are available. In this country, such preparations are virtually unavailable, if not illegal. However, we should not overlook the fact here that flavonoids are absorbed from the human gut into the blood, and thus may cause similar pharmacological effects (Middleton). Ursolic acid, oleanolic acid, chlorogenic and caffeic acids, sorbitol, fructose, harnic acid, adenine, and guanine (Bersin & Müller, Braasch & Bienroth, Nikolov & Ivanov) were isolated in the 1950s, but showed no activity on either the vessels or heart. Choline and acetylcholine were also isolated, but these are, for the most part, ubiquitous in higher plants (Sajner). According to Zeylstra (1983), the hawthorn preparations are most active when the whole plant extract is used, not an isolated fraction. Weiss, a German doctor with nearly 40 years of clinical experience with herbal remedies, says,"It is obvious that the actions of the individual elements (of hawthorn) are not merely additive or synergic, but that genuine potentiation occurs. So the role of these minor constituents may be to support the more active and unique compounds. For instance, a glyceroethanolic extract of the buds of C. laevigata has demonstrated greater cardioactivity than any individual constituent tested (Ficarra, et al., 1984b). 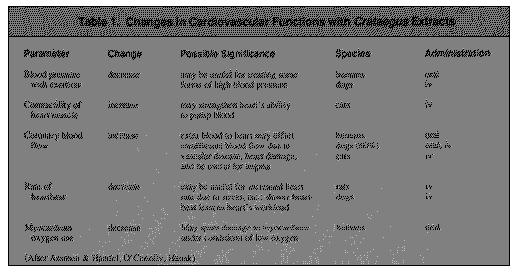 [For those with an abnormal interest in this early work on C. laevigata and C. monogyna, the original references can be found in Sajner & Veris (1963), Madaus, List & Hörhammer, and Ammon & Handel (1982 a,b).]
Recent Work (1960 to 1989)
Modern work on hawthorn extracts -- both commercial preparations and extracts of C. laevigata, C. monogyna, and to a lesser extent C. pentagyna -- have focused on two constituent groups: the flavonoids, and, more recently, several amines (which appear not to be active).
All vascular plants contain flavonoids, and hawthorn species are particularly rich in them, so it is not surprising that they have received a strong research emphasis. Some introductory information about flavonoids is given in Table 2.
[For those with an abnormal interest in this early work on C. laevigata and C. monogyna, the original references can be found in Sajner & Veris (1963), Madaus, List & Hörhammer, and Ammon & Handel (1982 a,b).]
Recent Work (1960 to 1989)
Modern work on hawthorn extracts -- both commercial preparations and extracts of C. laevigata, C. monogyna, and to a lesser extent C. pentagyna -- have focused on two constituent groups: the flavonoids, and, more recently, several amines (which appear not to be active).
All vascular plants contain flavonoids, and hawthorn species are particularly rich in them, so it is not surprising that they have received a strong research emphasis. Some introductory information about flavonoids is given in Table 2.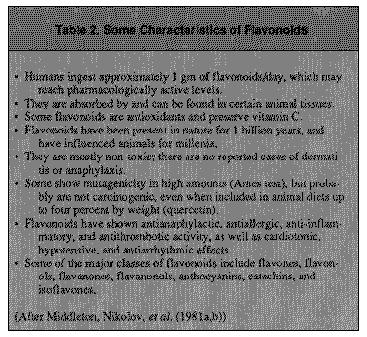 Flavonoids are bio-active plant pigments that are ubiquitous in higher plants and have a basic skeleton containing two aromatic C6 rings connected by three carbon atoms (Fig. 1). The first work on the flavonoids of C. laevigata and C. monogyna was conducted in 1953, when hyperoside, vitexin-4'-L-rhamnoside, quercetin, and vitexin were isolated by Kranen-Fiedler (Kowalewski & Mrugasiewicz). Since then, at least 30 more flavonoids have been isolated from these plants.
The classes of flavonoids that have been particularly well studied in hawthorn and have shown activity are flavone derivatives such as hyperoside and vitexin-4'-O-rhamnoside; oligomeric procyanidins (with varying degrees of polymerization); polymeric procyanidins; and the catechin l-epicatechin. Hawthorn fruits, as well as the leaves, contain catechin polymers, called condensed tannins, which account for the astringent effect noted by Gerard in the late 1500s.
Colorless condensed tannins can be transformed to phlobaphenes which have a bright red color. These "tannin reds," as they are sometimes called, have been ascribed cardioactive properties. List & Hörhammer mention that these red, crystalizable pigments (found mainly in the fruits, and to a lesser extent in the autumn leaves) have the same activity as pure anthocyanins, i.e., they have a tonic effect on the cardiac muscles, are negatively chronotropic and dromotropic, and also show the bradycardiac effect commonly noted for Crataegus which is supported in a study by Hahn, et al.
A list of the specific flavones, anthocyanins, and catechins that have been isolated and characterized, including ones that show activity, is presented in Table 3, pages 30-32.
The major flavonoids in Crataegus preparations are vitexin-2"rhamnoside, rutin, and hyperoside in flowers, with the addition of vitexin in the leaves (Tittel, G. & Wagner, 1982). One commercial preparation containing a mixture of total flavonoids has also been tested for activity (Crataemon). Other tested fractions include a preparation of purified triterpenic acids, unpurified triterpenic acids, oleanolic, oleanolic acids, and a fraction of total saponins.
Additional Notes on Pharmacology:
1."High doses of Crataegus agents lead to a decrease in cardiac output, low dosages increase it."
2."Lowers pathologically increased pyruvic and lactic acid levels" (which may be increased after heart damage).
3."[causes]...a decrease in heart frequency along with heightened systolic discharge and cardiac output after O(2)-deficit respiration of a healthy person and the prevention of ECG-alterations due to hypoxia."
(Adapted from List & Hörhammer)
CLINICAL APPLICATIONS Since the late 19th century, hawthorn has been used successfully for various heart diseases, including angina pectoris, functional heart disease, arrhythmia, early manifestations of circulatory insufficiency of advanced age, and as a heart tonic to regulate circulation. It has also found use for menopausal symptoms, arteriosclerosis, and as a diuretic (Madaus). Recently, the beneficial effects of a hawthorn preparation on the heart and circulation are supported with two placebo-controlled, crossover double-blind studies in humans (O'Connolly, et al. and Iwamoto, et al.). Iwamoto's group studied the effects of an alcoholic extract of the fruits and leaves of C. monogyna and C. laevigata compared with placebos in 120 people with sage 2 or 3 loss of cardiac output. "The New York Heart Association proposed the sages of loss of cardiac output. Stage 1 loss of capacity means that the patient is symptom-free when at rest or during treatment. Sage 2 patients have loss of capacity with medium effort and more, stage 3 loss of capacity means that minor effort results in obvious labored or difficult breathing and stage 4 patients experience symptoms when at rest." The researchers clearly demonstrated an improvement in subjective symptoms, when compared with the placebo group, especially with shortness of breath and palpitations. Cardiac function was said to be improved.
One of hawthorn's primary applications is to support the effect of digitalis, and to serve as a substitute where digitalis cannot be tolerated or where side effects need to be avoided (Madaus).
About this effect, List and Hörhammer add:It is reasonable to combine digitalis and Crataegus, especially because the addition of hawthorn to digitalis or strophanthin speeds up recompensation, particularly in older patients, and reduces the intolerance phenomena or unpleasant side effects, such as nausea.
In modern European medicine, Crataegus preparations are widely used for chronic or light cases of cardiovascular diseases. Steinegger & Hänsel emphasize that:
Cratae gus preparations are not specific drugs for treatment of acute illnesses. They are first and foremost a preventative drug to slow down the aggravation of beginning cardiovascular damage.
Hager's Handbook, one of the most complete modern compilations on medicinal plants, lists interesting (and representative) clinical uses for hawthorn preparations (List & Hörhammer). Although the chemistry and pharmacology are somewhat dated, the uses are still pertinent and are summarized in Table 4, along with additional information by Zeylstra (1983), an experienced British clinical herbalist.
A more conservative view of the scope of hawthorn's application is represented by this excerpt from a recent German monograph drafted by Commission E (Bundesanzeiger #1, Jan. 2, 1984):
- reduction in heart function (NYHA stages I or II)
- uneasiness and oppressed feeling of the heart
- not yet digitalized heart
- light forms of bradycardic arrhythmia
Flavonoids are bio-active plant pigments that are ubiquitous in higher plants and have a basic skeleton containing two aromatic C6 rings connected by three carbon atoms (Fig. 1). The first work on the flavonoids of C. laevigata and C. monogyna was conducted in 1953, when hyperoside, vitexin-4'-L-rhamnoside, quercetin, and vitexin were isolated by Kranen-Fiedler (Kowalewski & Mrugasiewicz). Since then, at least 30 more flavonoids have been isolated from these plants.
The classes of flavonoids that have been particularly well studied in hawthorn and have shown activity are flavone derivatives such as hyperoside and vitexin-4'-O-rhamnoside; oligomeric procyanidins (with varying degrees of polymerization); polymeric procyanidins; and the catechin l-epicatechin. Hawthorn fruits, as well as the leaves, contain catechin polymers, called condensed tannins, which account for the astringent effect noted by Gerard in the late 1500s.
Colorless condensed tannins can be transformed to phlobaphenes which have a bright red color. These "tannin reds," as they are sometimes called, have been ascribed cardioactive properties. List & Hörhammer mention that these red, crystalizable pigments (found mainly in the fruits, and to a lesser extent in the autumn leaves) have the same activity as pure anthocyanins, i.e., they have a tonic effect on the cardiac muscles, are negatively chronotropic and dromotropic, and also show the bradycardiac effect commonly noted for Crataegus which is supported in a study by Hahn, et al.
A list of the specific flavones, anthocyanins, and catechins that have been isolated and characterized, including ones that show activity, is presented in Table 3, pages 30-32.
The major flavonoids in Crataegus preparations are vitexin-2"rhamnoside, rutin, and hyperoside in flowers, with the addition of vitexin in the leaves (Tittel, G. & Wagner, 1982). One commercial preparation containing a mixture of total flavonoids has also been tested for activity (Crataemon). Other tested fractions include a preparation of purified triterpenic acids, unpurified triterpenic acids, oleanolic, oleanolic acids, and a fraction of total saponins.
Additional Notes on Pharmacology:
1."High doses of Crataegus agents lead to a decrease in cardiac output, low dosages increase it."
2."Lowers pathologically increased pyruvic and lactic acid levels" (which may be increased after heart damage).
3."[causes]...a decrease in heart frequency along with heightened systolic discharge and cardiac output after O(2)-deficit respiration of a healthy person and the prevention of ECG-alterations due to hypoxia."
(Adapted from List & Hörhammer)
CLINICAL APPLICATIONS Since the late 19th century, hawthorn has been used successfully for various heart diseases, including angina pectoris, functional heart disease, arrhythmia, early manifestations of circulatory insufficiency of advanced age, and as a heart tonic to regulate circulation. It has also found use for menopausal symptoms, arteriosclerosis, and as a diuretic (Madaus). Recently, the beneficial effects of a hawthorn preparation on the heart and circulation are supported with two placebo-controlled, crossover double-blind studies in humans (O'Connolly, et al. and Iwamoto, et al.). Iwamoto's group studied the effects of an alcoholic extract of the fruits and leaves of C. monogyna and C. laevigata compared with placebos in 120 people with sage 2 or 3 loss of cardiac output. "The New York Heart Association proposed the sages of loss of cardiac output. Stage 1 loss of capacity means that the patient is symptom-free when at rest or during treatment. Sage 2 patients have loss of capacity with medium effort and more, stage 3 loss of capacity means that minor effort results in obvious labored or difficult breathing and stage 4 patients experience symptoms when at rest." The researchers clearly demonstrated an improvement in subjective symptoms, when compared with the placebo group, especially with shortness of breath and palpitations. Cardiac function was said to be improved.
One of hawthorn's primary applications is to support the effect of digitalis, and to serve as a substitute where digitalis cannot be tolerated or where side effects need to be avoided (Madaus).
About this effect, List and Hörhammer add:It is reasonable to combine digitalis and Crataegus, especially because the addition of hawthorn to digitalis or strophanthin speeds up recompensation, particularly in older patients, and reduces the intolerance phenomena or unpleasant side effects, such as nausea.
In modern European medicine, Crataegus preparations are widely used for chronic or light cases of cardiovascular diseases. Steinegger & Hänsel emphasize that:
Cratae gus preparations are not specific drugs for treatment of acute illnesses. They are first and foremost a preventative drug to slow down the aggravation of beginning cardiovascular damage.
Hager's Handbook, one of the most complete modern compilations on medicinal plants, lists interesting (and representative) clinical uses for hawthorn preparations (List & Hörhammer). Although the chemistry and pharmacology are somewhat dated, the uses are still pertinent and are summarized in Table 4, along with additional information by Zeylstra (1983), an experienced British clinical herbalist.
A more conservative view of the scope of hawthorn's application is represented by this excerpt from a recent German monograph drafted by Commission E (Bundesanzeiger #1, Jan. 2, 1984):
- reduction in heart function (NYHA stages I or II)
- uneasiness and oppressed feeling of the heart
- not yet digitalized heart
- light forms of bradycardic arrhythmia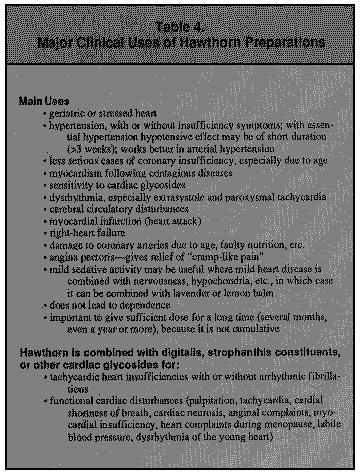
 In Italy, hawthorn preparations are used more for mild anxiety and other nervous disturbances than for heart ailments (Loggia, et al.).
In modern allopathic clinical practice, especially in Germany, early digitalization of the geriatric heart is not advised. This used to be regularly practiced, though partly because of increased acceptance of hawthorn preparations is now less common. Only when there are clear signs of cardiac insufficiency and tachycardiac auricular fibrillation is digitalis recommended (Meier). The use of hawthorn extracts are encouraged in these cases because studies indicate that digitalis can cause unwanted symptoms of poisoning in 20-30% of the patients receiving it.
Follath (1986, 1989) reports side effects with two other commonly-prescribed drug therapies for declining geriatric hearts -calcium antagonists and beta blockers. Another important reason for emphasizing Crataegus over synthetic drugs, where appropriate, is the possible beneficial effect of Crataegus on the strength of the heart. Meier puts it succinctly:
"Numerous pharmacological investigations have shown that Crataegus -- in contrast to, for example, the digitalis glycosides' negatively chronotropic and positively inotropic effects -- develops effects on all levels beneficial to a beginning cardiac insufficiency. On the one hand this is achieved in the heart by an increase in coronary flow and in myocardiac circulation, and on the other by a decrease in peripheral vascular resistance."
Weiss gives clear clinical indications for the use of hawthorn preparations.
1. Senile hearts. "The anginal symptoms of coronary disease in particular tend to disappear with Crataegus therapy. Recurrences can be largely prevented."
2. Hypertensive hearts, in failure or not, mainly to maintain heart muscle in good condition.
3. "Weakness of myocardium after infectious diseases such as pneumonia, influenza, diptheria, scarlet fever, etc. Possibly also adding Crataegus to digitalis or strophanthin medication to optimize their effect."
4. Cardiac arrhythmias, mainly extrasystoles.
5. "In middle-aged patients showing the first signs of coronary involvement..."
6."...follow-up therapy of myocardial infarction..."
He adds the following suggestions:
1. "...treatment has to be long-term [at least several months]. Little or nothing may be expected from short-term use, except for...arrhythmias [extrasystoles]."
2. "Patients will again and again speak of subjective improvement.."
3. Crataegus preparations are not for hospital practice, because "instant effects have to be achieved." Crataegus is more for general practice, and it is "completely safe for long-term use."
4. The dose is 30 to 40 drops three times daily to begin and "...later as maintenance therapy, morning and night." In severe cases, a "teaspoonful of the extract can safely be taken at once, two or three times daily, though only for a limited period, up to some weeks if necessary."
In Italy, hawthorn preparations are used more for mild anxiety and other nervous disturbances than for heart ailments (Loggia, et al.).
In modern allopathic clinical practice, especially in Germany, early digitalization of the geriatric heart is not advised. This used to be regularly practiced, though partly because of increased acceptance of hawthorn preparations is now less common. Only when there are clear signs of cardiac insufficiency and tachycardiac auricular fibrillation is digitalis recommended (Meier). The use of hawthorn extracts are encouraged in these cases because studies indicate that digitalis can cause unwanted symptoms of poisoning in 20-30% of the patients receiving it.
Follath (1986, 1989) reports side effects with two other commonly-prescribed drug therapies for declining geriatric hearts -calcium antagonists and beta blockers. Another important reason for emphasizing Crataegus over synthetic drugs, where appropriate, is the possible beneficial effect of Crataegus on the strength of the heart. Meier puts it succinctly:
"Numerous pharmacological investigations have shown that Crataegus -- in contrast to, for example, the digitalis glycosides' negatively chronotropic and positively inotropic effects -- develops effects on all levels beneficial to a beginning cardiac insufficiency. On the one hand this is achieved in the heart by an increase in coronary flow and in myocardiac circulation, and on the other by a decrease in peripheral vascular resistance."
Weiss gives clear clinical indications for the use of hawthorn preparations.
1. Senile hearts. "The anginal symptoms of coronary disease in particular tend to disappear with Crataegus therapy. Recurrences can be largely prevented."
2. Hypertensive hearts, in failure or not, mainly to maintain heart muscle in good condition.
3. "Weakness of myocardium after infectious diseases such as pneumonia, influenza, diptheria, scarlet fever, etc. Possibly also adding Crataegus to digitalis or strophanthin medication to optimize their effect."
4. Cardiac arrhythmias, mainly extrasystoles.
5. "In middle-aged patients showing the first signs of coronary involvement..."
6."...follow-up therapy of myocardial infarction..."
He adds the following suggestions:
1. "...treatment has to be long-term [at least several months]. Little or nothing may be expected from short-term use, except for...arrhythmias [extrasystoles]."
2. "Patients will again and again speak of subjective improvement.."
3. Crataegus preparations are not for hospital practice, because "instant effects have to be achieved." Crataegus is more for general practice, and it is "completely safe for long-term use."
4. The dose is 30 to 40 drops three times daily to begin and "...later as maintenance therapy, morning and night." In severe cases, a "teaspoonful of the extract can safely be taken at once, two or three times daily, though only for a limited period, up to some weeks if necessary."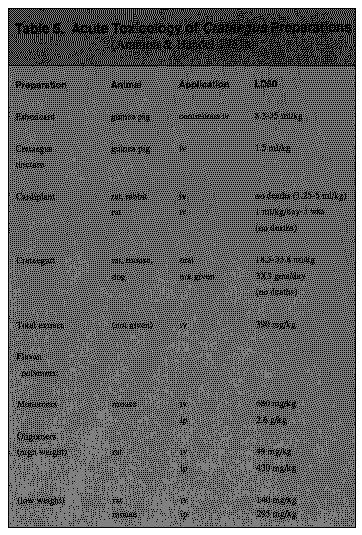 TOXICITY
In over 100 years of clinical use, there have been no reported cases of toxicity with hawthorn preparations. Animal studies show no acute toxicity even with extremely high doses (Table 5), though chronic and sub-chronic toxicity must still be evaluated with modern methods. It would also be desirable to know if hawthorn extracts show any mutagenicity, carcinogenicity, or teratogenicity, Unfortunately, these data are not available at this time and cannot be gained from an evaluation of the existing studies. We do know that the flavonoid quercefin shows mutagenicity on the Ames test, though it occurs in low concentration in hawthorn extracts (Schimruer).
According to Ammon & Händel (1981a), toxicity to the fetus is of little concern since hawthorn preparations are usually given to elderly patients. Hypersensitivity to the fruit has been reported, although it is rare (Steinman).
PHARMACY
Preparations
Crataegus fruits contain less of the major flavones (vitexin-2-"rhamnoside, rutin, and hyperoside) found in the flowers and leaves. The flowers contain the most hyperoside, the leaves the most vitexin-2"-rhamnoside. For this mason manufacturers often mix either two or three of these respective parts (Tittel & Wagner, 1982). One study reported a glycero-ethanolic extract of the young shoots to be most active (Costa, et al., Occhuito, et al.). Table 8 shows the content of chlorogenic acid, vitexin, vitexin-4"-rhamnoside, and hyperoside in the flowers, leaves, and buds of C. laevigata in different menstruums (from Ficarra, et al., 1984b).
High Pressure Liquid Chromatography (HPLC) is needed to determine whether a given batch of hawthorn contains sufficient quantities of flavonoids or other active components, for which complete methods are reviewed by Tittel and Wagner (1982) and
TOXICITY
In over 100 years of clinical use, there have been no reported cases of toxicity with hawthorn preparations. Animal studies show no acute toxicity even with extremely high doses (Table 5), though chronic and sub-chronic toxicity must still be evaluated with modern methods. It would also be desirable to know if hawthorn extracts show any mutagenicity, carcinogenicity, or teratogenicity, Unfortunately, these data are not available at this time and cannot be gained from an evaluation of the existing studies. We do know that the flavonoid quercefin shows mutagenicity on the Ames test, though it occurs in low concentration in hawthorn extracts (Schimruer).
According to Ammon & Händel (1981a), toxicity to the fetus is of little concern since hawthorn preparations are usually given to elderly patients. Hypersensitivity to the fruit has been reported, although it is rare (Steinman).
PHARMACY
Preparations
Crataegus fruits contain less of the major flavones (vitexin-2-"rhamnoside, rutin, and hyperoside) found in the flowers and leaves. The flowers contain the most hyperoside, the leaves the most vitexin-2"-rhamnoside. For this mason manufacturers often mix either two or three of these respective parts (Tittel & Wagner, 1982). One study reported a glycero-ethanolic extract of the young shoots to be most active (Costa, et al., Occhuito, et al.). Table 8 shows the content of chlorogenic acid, vitexin, vitexin-4"-rhamnoside, and hyperoside in the flowers, leaves, and buds of C. laevigata in different menstruums (from Ficarra, et al., 1984b).
High Pressure Liquid Chromatography (HPLC) is needed to determine whether a given batch of hawthorn contains sufficient quantities of flavonoids or other active components, for which complete methods are reviewed by Tittel and Wagner (1982) and 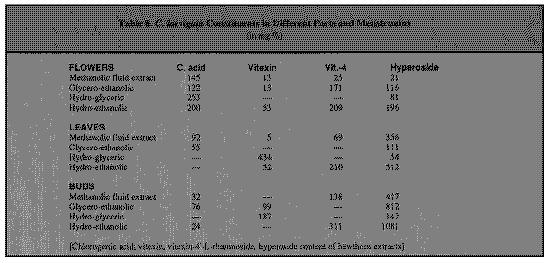 Table 3. The Major Consitutents and Activity of Crataegus spp.
((*) C. laevigata unless specified otherwise)
Constituent group & Constituent Activity (If Known)
Aromatic Carboxylic acids
not studied in Crataegus
(phenolic derivatives)
chlorogenic, caffeic acids (1)
(1,2,3)
Sterols
not studied in Crataegus
beta-sitosterol (1) 0.51-0.62 ,
(fl) 0.65-0.78 (4,4)
Pentacyclic Triterpenes
no effect (5,6); - chronotropic, +
oleanolic acid, ursolic acid, inotropic, and coronary dilation
effects
acantolic acid, neotegolic acid, (7); antiarrhythmic (8)
2-alpha-hydroxy-oleanic acid
(syn. crataelogic acid) (l,f)
(total in leaves,0.5-1.4%; fruit
0.3-1.4%; blossoms, 0.7-1.2%)
(3,9,10,11)
Flavonoids:
Flavones (3,12,13,14,15)
mixture of flavones orally in mice show
hyperoside (hyperin) (1)
weak sedative CNS effect (in dose = to
11
vitexin (1)
gms in a 135 lb rat), humans more
vitexin-rhamnoside (1)
sensitive to sedatives (16); hyperoside
vitexin-4'-L-rhamnoside(main one) iv to dogs lowered blood pressure prob.
vitexin-4'-L-rhamno-d-glucoside from peripheral vasodilat., no effect
on
vitexin-4'-7-di-d-glucoside
heart (17);
rutin
quercetin-3-rhamno-galactoside
2.2% total flavonoid standardized oral dose in rats w/ placebo group
extract (according to the 9th strongly potentiated protective effects
German Pharmacopeia -- DAB 9) of garlic against isoprenaline-induced
heart damage (18)
(*) Crataegus monogyna
See Crataemon section
total flavonoid content 1.8% (19)
or 4.4%, 0.64% hyperoside (20)
vitexin-4'-O-rhamnosi(deacylated)
(main constituent) (21);
vicenins-1,2,3; schaftoside;
iso-, neo- and neoiso-schaftoside
(22); quercetin, crateside,
luteolin-7-O-glycoside, orientin,
iso-orientin (Nikolov, et al.,
1982) Catechins
(6)
(+)-catechin (11)
(-)-epicatechin (23,24,25)
(*) heptahydroxyflavan glycoside iv, ia: increase in circulation,
(26) from "Eurhyton" (a
(27); iv in cats: hypotensive, +
polycondensation product of inotropic (28)
flavan units)
"flavan polymer fraction"
Proanthocyanidins (syn.
procyanidins, pycnogenol)
pycnogenol from pine-needle extract is
flavan dimers, hexamers,
sold on the American health food market
oligomers,polymers;total,1-3�9) as an oxygen radical scavenger
oligomeric proanthocyanidins (30) (anti-oxidant) (author's observation);
cardioactive in vitro (7)
cats, mice, iv, ip: lowers blood
pressure & body temp., CNS sedative
(31,32)
oligomeric procyanidin
long-term oral dose in dogs led to up
70%
(standardized -- (OPC)
increase in blood flow in left
ventricle (33)
polymers of proanthocyanidins showed broad spectrum of antibiotic
(condensed tannins)
properties (34)
Commercial preparations
(*) Esbericard (water extr.
iv, ia in dogs: vasodilation peripheral
of flowers and leaves +(flowers?) resistance lowered (35, 36, 37)
(1:3)standardized to 8�ondensed uncontrolled study with 40 older heart
flavans 1-catechin part of total patients showed clinical improvement,
activity
even when previously digitialized (38)
(*)Crataegutt(EtOH extract of fl, guinea pig heart in vitro: increase in
1 of C. monogyna + C. laevigata, blood flow, potentiated pos. inotropic
standardized to 200 mg
effects of digitalis, etc. (39); oral
procyanidins/100 ml)
administration in dogs led to increase
in blood flow to left ventricle of heart (40); oral administration in rabbits significantly reduced anoxic-induced recovery time of heart muscle + refs. (41); oral dose in dogs
led to 25-39% increase (42); oral dose vs. placebo in 36 humans w/decreased
heart performance benefited heart and subjective improvement (43); controlled d-blind study w/oral application showed increased coronary perfusion and economizing of myocardial oxygen consumption, normalization of ECG; treatment suitable for NYHA stages I and II not yet needing nitrates, beta-receptor blocking agents and Ca antagonists (44) (*) Crataemon (total flavonoid in small amounts, reduces oxygen mixture from C. monogyna (flowers consumption,activating respiration in and leaves) contains 19 heart mitochondria in vitro, possibly
flavonoids:(47) due to a zinc-flavonoid complex (45); iv dose in dogs raises coronary blood flow (46)[contains alcohol?];1 oral administration in rats in a controlled study led to increased vascularization in heart after induced infarction quercetin, kaempferol, hyperoside, crataeside, glogoside, rutin, spiraeoside, quercetin-3-O-rhamno-galactoside, luteolin-7-O-glucoside+ 12 flavone C-glycosides (vitexin,
isovitexin,orientin, isoorientin, monoacetyl-isoorientin, rhamnosyl-vitexin, 2 C-glycosides of apigenin and others (l,fl) (28,29) Purine (xanthine) derivatives no data
adenosine, adenine, guanine, uric acid (1) (3,11,48) Saponins (total fraction) from no data C. pentagyna (49) Amines (3) ethylamine, dimethylamine,
show + inotropic effect in
vitrotrimethylamine,isobutylamine (guinea pig papillary muscle) (50)
isobutylamine,
isoamylamine, ethanolamine,
beta-phenylethylamine, choline,
acetylcholine (1) phenethylamine,
o-methoxyphenethylamine, tyramine
(fl) polyamines(spermindine)(11)
Amino Acids (51)
Total free AA:leaves(22.8 mmol/kg flowers considered to be a good
dry weight), flowers (52.3),
source of cardioactive compounds (52)
fruits (6.3)
Misc. (3,11)
Vitamin C (1 = 0.18%, 0.14-0.25% no data
in C. rnonogyna)
Essential oil (1) 0.157%
--
Sorbitol
--
Amygdalin (1=0.15%)
--
Pectin
--
Aesculin (in the bark)
--
Mineral salts, especially sodium --
Whole plant extract
pos. inotropic -- guinea pig heart
Water decoction
muscle (53); iv in rats showed
dose-dependant hypotensive effect
(54)
Extracts of Crataegus pinnatifida among 4 plants tested, induced
greatest SOD activity in red blood
cells in vitro (55)
Hawthorn in Chinese Medicine
C. pinnatifida Bge. var.
show cardiotonic activity in animals
major N.E..Br.,C. pinnatifidaBge. in vitro and in vivo; in humans
or C. cuneata Sieb. et Zucc.
(all studies uncontrolled) extracts lowered serum cholesterol, relieved symptoms of angina, hypertension, palpitations, insomnia, coronary insufficiency, dyspepsia, successfully treated bacillary dysentery and enteriris, hepatitis,and pyelonephritis (56)
Footenootes - Table 3
(1.) Hockerts, T. & G. Mülke. 1955. Studies on the coronary effect of aqueous extracts of Crataegus. Arzneim.-Forsch. 5: 755-7.
(2.) Ficarra, P., et el. 1984a. High-performance liquid chromatography of flavonoids in C. laevigata L. I:reversed-phase high pressure liquid chromatography. Il Farmaco-Ed. Pr. 39: 148-57.
(3.) List & Hörhammer, opus cited.
(4.) Bersin, T. &A. MÜller. 1952. Concerning the constituents of Crataegus oxyacantha. II: betasitosterin and oleanic acid. Helv. Chim. Acta 35: 1891-1895.
(5.) Dörner, J. & H.J. Kuschke. 1955. Do Crataegus triterpenic acids (Crataogus acids) possess a pharmacodynamic effect? Archiv fÜr exper. Pathologie and Pharmacologie 225:144.
(6.) Nikolov, et al. (1981), opus cited.
(7.) Occhiuto, F., et al. 1986. Study comparing the cardiovascular activity of shoots, leaves and flowers of C. laevigata L. II: Effect of extracts and pure isolated active principles on the isolated rabbit heart. Plantes Mtd. Phytother. 20: 52-63.
(8.) Occhiuto, F., et al. 1986. Study comparing the cardiovascular activity of young shoots,leaves and flowers of C. laevigata L. I: Electrical activity and arterial pressure in the rat. Plantes Med. Phytother. 20: 37-51.
(9.) Bersin, T. & MÜller. 1951. Concerning the constituents of Crataegus oxyacantha L. I: ursolic acid. Helv. Chim. Acta 34: 1868-72.
(10.) Braasch & Bienroth, opus cited.
(11.) Steinegger & Hänsel, opus cited.
(12.) Ficarra, et al. (1984a), opus cited.
(13.) Fisel, J. 1965. New flavonoids from Crataegus. I: Isolation of an acetylated vitexin-4'rhamnoside from C. monogyna L. Arzneim.-Forsch. 15: 1417-21.
(14.) Fisel, J. 1966. New flavonoids from Crataegus. II: Isolation of a mixture of rutin and quercetin-3-rhamnoglactoside from C. monogyna L. (xx CH journal name coming).
(15.) Kowalewski, Z. & K. Mrugasiewicz. 1968. New flavanonheterosides in C. phenophyrum. Planta Med. 19:311-17.
(16.) Loggia, R.D., et el. 1983. Depressive effect of C. laevigata L. on central nervous system in mice. Sci. Pharm. 51: 319-24. (English).
(17.) Lievre, M., et al. 1985. Assessment in the anesthetized dog of the cardiovascular effects of a pure extract (hyperoside) from hawthorn. Ann. Pharm. Fran. 43:471-7.
(18.) Ciplea, A.G. & K.-D. Richter. 1988. The protective effect of Allium sativum and Crataegus on isoprenaline-induced tissue necroses in rats. Arzneim.-Forsch. 38: 1583-92. (English).
(19.) Nikolov, N. & V. Ivanov. 1969. Flavonoid composition of C. monogyna. I:Isolation of a flavonoid mixture from the leaves. Farmatsiya 19: 32-7. (Chem. Ab. 73: 32285v).
(20.) Simova, M. & T. Pangarova. 1983. Flavonoid determination in hawthorn. Pharmazie 38: 791-2.
(21.) Pietea, P., et al. 1986. Isocratic liquid chromatographic method for the simultaneous determination of Passiflora incarnata L. and C. monogyna flavonoids in drugs. J. of Chrom. 357: 233-8.
(22.) Nikolov, N., et al. 198 lb. Di-C-glycosylflavones from C. monogyna. Phytochem. 20: 2780-1.
(23.) Rewerski, W. & S. Lewak. 1967. Some pharmacological properties of flavanpolymers from hawthorn (C. Laevigata). Arzneim.-Forsch. 17: 490.
(24.) Rewerski, W., et al. 1971. Some pharmacological properties of oligomeric procyanidins isolated from hawthorn (C. Laevigata). Arzneim.-Forsch. 21: 886-7.
(25.) Schwabe, W. & R. Neu. 1960. Pharmacological examination of a substance from Crataegus. Arzneim.-Forsch. 10: 60.
(26.) Bersin, T. 1955. Studies on the ingredients of Crataegus oxycantha L. Arzneim.-Forsch. 5:490.
(27.) Engelking, R. & F. Willig. 1958. The cardiac and circulatory action of a water-soluble Crataegus ingredient (heptahydroxyflavanglycoside) in dogs. Arzneim.-Forsch. 8: 39-42.
(28.) Rewerski, W. & Lewak, S. 1967. Some pharmacological properties of flavan polymers isolated from hawthorn (C. laevigata). Arzneim.-Forsch. 17: 490-1.
(29.) Steinegger, E. & R. Hänsel. 1988. Handbook of Pharmacognosy and Phytopharmacy. New York: Springer-Verlag. (German).
(30.) Hö1zl, J. & A. Strauch. 1977. Investigation on the biosynthesis of oligomer procyanidins of Crataegus. Planta Med. 32: 141-53.
(31.) Reweeski, W., et al. Some pharmacological properties of oligomeric procyanidin isolated from hawthorn (C. laevigata). Arzneim.-Forsch. 21: 886-8.
(32.) Rewerski, et al. (1971), opus cited.
(33.) Roddewig, C. & H. Hensel. 1977. Reaction of local myocardial blood flow in non-anesthetized dogs and anesthetized cats to oral and parenteral application of a Crataegus fraction (oligomere procyanidins). Arzneim.-Forsch. 27: 1407-10.
(34.) Porter, L.J. 1986. Proanthocyanidin polymers (PAP) have broad-spectrum antibiotic properties. Aust. J. Chem. 39: 557-62.
(35.) Kovach, A.G.B., et al. Effects of an extract obtained from C. laevigata on coronary blood flow in dogs. Arzneim.-Forsch. 9: 378-9.
(36.) Schwabe, W. & R. Neu. Pharmacological investigations of a new substance isolated from Crataegus. Arzneim.-Forsch. 10: 60-1.
(37.) Ammon & Händel (1981c).
(38.) Berker, R. 1984. Therapy in heart insufficiency where glycosides are not required. Medwelt 35: 1567-9.
(39.) Trunzler, G. & E. Schuler. Comparative studies on the effects of a Crataegus extract, digitoxin, digoxin and g-strophanthin in the isolated heart of homoiothermals. Arzneim.-Forsch. 12: 198-202.
(40.) Mäves, W.H. & H. Hensel. 1974. Changes in local myocardial blood flow following oral administration of a Crataegus extract to non-anesthetized dogs. Arzneim.-Forsch. 24: 7835.
(41.) Kanno, T., et al. 1976. Reduction of the hypoxia-induced depression in the intracellular electrical activity of the ventricular muscle fibers of the rabbit fed on food containing Crataegutt. Jap. Heart J. 17: 512-520.
(42.) Mävers, W.H. & H. Hensel. 1974. Changes in local blood flow after oral application of a Crataegus extract in un-narcotised dogs. Arzneim.-Forsch. 24: 783.
(43) O'Connolly, M., et al. Treatment of decreasing cardiac performance (NYHA stages I to II) in advanced age with standardized Crataegus extract. Fortschr. Med 104: 805-8.
(44.) Hanak, Th. & M.H. Bruckel. 1983. Treatment of mild stable forms of angina pectoris with a standardized Crataegus extract. Therapiewoche 33/34: 4331-3.
(45.) Ivancheva, E., et al. 1976. Effect of Crataemon on the respiration of isolated mitochondria. Acta Phys. Pharm. Bulg. 2: 35-40.
(46.) Taskov, M. 1977. On the coronary and cardiotonic action of Crataemon. Acta Phys. Pharm. Bulg. 3: 53-57. (English).
(47.) Guendjev, Z. 1977. Experimental myocardial infarction of the rat and stimulation of the revascularization by the flavonoid drug Crataemon. Arzneim.-Forsch. 27:1576-9. (English).
(48.) Kranen-Fiedler, U. 1955. Ingredients obtained from Crataegus. Arzneim.-Forsch. 5: 757-8.
(49.) Gusseinow, D.J. 1965. On the pharmacology of the total saponins from C. pentagyna W. et K. Farmakol. i Toksikol. 28: 172.
(50.) Wagner, H. & J. Grevel. 1982. Cardioactive drugs IV: Cardiotonic amines from C. Oxyacantha. Planta Med. 45: 98-101.
(51.) Kiseleva, T.L., et al. 1989. Amino acid composition of the flowers of pharmacopoeial and non-pharmacopoeial species of Crataegus L. Rastitel'nye Resursy 25: 145-54.
(52.) Kiseleva, T.L., et al. The free amino acid composition in different organs of C. oxyacantha (Poir.) DC. 1989. Rastitel'nye Resursy 25: 92-7.
(53.) Vogel, G. 1975. Predictability of the activity of drug combinations -- yes or no? Arzneim.Forsch. 25: 1356-65.
(54.) Abdul-Ghani, A.-S., et el. 1987. Hypotensive effect of C. oxyacantha. Int. J. Crude Drug Res. 25: 216-20.
(55.) Dai, Y.R., et al. 1987. Effect of extracts of some medicinal plants on superoxide dismutase activity in mice. Planta Med. 53: 309-10.
(56.) Chang, H.-M. & P. P-H. But. 1986. Pharmacology and Applications of Chinese Materia Medica, 2 vols. Philadelphia: World Scientific.
References
Alcock, R.H. 1876. Botanical Names for English Readers. London: L. Reeve & Co.
Alleyne, J. 1733. The New English Dispensatory. London: Tho. Astley.
Ammon, H.P.T. & M. Händel. 1981a. Crataegus, toxicology and pharmacology. Part I. toxicology. Planta Med. 43: 105-120.
Ammon, H.P.T. & M. Händel. 1981b. Crataegus, toxicology and pharmacology. Part II: pharmacodynamics. Planta Med. 43:313-322 (with references).
Ammon, H.P.T. & M. Händel. 1981c. Crataegus, toxicology and pharmacology. Part III: pharmacodynamics and pharmacokinetics. Plante Med. 43: 209-239.
Anon. 1927. Facsimile Reproductions of the Principal Labels of Specific Medicines. Cincinnati: Lloyd Brothers Pharmacists, Inc.
Bailey, L.H. 1939. The Standard Cyclopedia of Horticulture. Vol. 1. New York: The Macmillan Company.
Bensky, D. & A. Gamble. 1986. Chinese Herbal Medicine: Materia Medica. Seattle: Eastland Press.
Braasch, W. & W. Bienroth. 1960. Peripheral circulatory effects of an aqueous extract from Crataegus in dogs. Arzneim.-Forsch. 10: 127-9.
Chekalinskaya, I.I., et al. 1985. Chemosystematic study of plants of the genus Crataegus. Referativnyi Zhurnal 9V548.
Cockayne, O. (ed.). 1864-6. Leechdoms, Wortcunning, and Starcraft of Early England. London:
Costa, R., et al. 1986. Comparative study of the cardiovascular activity of young shoots, leaves and flowers of C. laevigata L. Part III. Protective action on the isolated rat heart against arrhythmogenic agents and arrhythmias induced by reperfusion. Plantes Med. Phytother. 20: 115-28.
Dirr, M.A. and C.W. Heuser, Jr. 1987. The Reference Manual of Woody Plant Propagation: From Seed to Tissue Culture. Athens, Georgia: Varsity Press, Inc.
Duncan, W.H. and M.B. Duncan. 1988. Trees of the Southeastern United States. Athens: University of Georgia Press.
Eggleston, W.W. 1908. The Crataegi of the Northeastern United States and Adjacent Canada. Rhodora 10 (113): 73-84.
Emerson, G.B. 1875. A Report on the Trees and Shrubs of Massachusetts. 2nd ed. Boston: Little Brown and Company.
Erichsen-Brown, C. 1979. Use of Plants for the Past 500 Years. reprint ed. 1989; Medicinal and other uses of North American Plants. New York: Dover Publication.
Everett, Thomas H. 1981. The New York Botanical Garden Illustrated Encyclopedia of Horticulture. Vol. 3. New York: Garland Publishing, Inc.
Flück, H. & H. Schwabe. 1968a. Investigation of herb conservation with C. monogyna in the temperature range 20-100 deg. C. Part I: Quantitative Measurements of flavon heterosides. Planta Med. 16: 257-68.
Flück, H. & H. Schwabe. 1968b. Investigation of herb conservation with C. monogyna in the temperature range 20-100 deg. C. Part II: Enzymatic Decomposition of Flavon Heterosides. Planta Med. 16: 377-87.
Frisk, G. 1949. A Middle English Translation of Macer Floridus de Viribus Herbarum. Cambridge: Harvard University Press.
Gerard, J. 1597. The Herbal or Generall Historie of Plantes....London: John Norton.
Gerard, J. 1633. The Herbal or General Historie of Plants....Revised and enlarged by T. Johnson, reprinted by Dover Publications, New York. 1975.
Gunther, R.T. 1933. The Greek Herbal of Dioscorides. Hafner Publishing Co. 1968.
Hahn, F., et al. 1960. Preparation and pharmacological investigation of a new therapeutic agent obtained from Crataegus oxyacantha. Arzneim-Forsch. 10:825.
Hanak, Th. 1983. Treatment of mild stable forms of angina pectoris with a standardized Crataegus extract. Therapiewoche 33/34: 4331-3.
Herbarium Apulei. 1481. Milano: Edizioni il Polifilo (1979).
Hooper, D. 1929. On Chinese medicine: drugs of Chinese pharmacies in Malaya. The Gardens' Bulletin 6:1-165.
Hort, A.F. 1948. Theophrastus Enquiry into Plants. Cambridge: Harvard University Press.
Hou, J.P. 1977. The Development of Chinese Herbal Medicine and the Pen-ts'ao. Comparative Medicine East and West 5 (2): 117-122.
Hsu, H.-Y., et el. 1986. Oriental Materia Medica. Long Beach: Oriental Healing Arts Institute.
Hsu, H.Y. et al. 1986. Oriental Materia Medica: A Concise Guide. Long Beach, CA: Oriental Healing Arts Institute.
Institutum Botanicum Pekinense Academiae Sinicae. 1974. Flora Reipublicae Popularis Sinicae Vol. 36. Rosaceae(1) (Chinese).
Iwamoto, M, et al. 1981. Clinical effect of Crataegutt in ischaemic heart disease and/or hypertensive origin. Planta Meal. 42: 1.
Jones, W.H.S. 1953. Pliny Natural History (23-79 AD). Cambridge: Harvard University Press.
Levey, M. & N. Al-Khaledy. 1967. The Medical Formulary of Al-Samarqandi. Philadelphia: University of Pennsylvania Press.
Liberty Hyde Bailey Hortorium, Staff of the. 1976. Hortus Third. NY: Macmillan, 1290 pp.
List, P.H. & L. Hörhammer. 1969-79. HagersHandbuch der Pharrnazeutischen Praxis, vols. 2-6a,b,c. New York: Springer-Verlag.
Little, E.L. 1980. The Audubon Society Field Guide to North American Trees. New York: Alfred A. Knopf.
Lloyd, J.U. 1917. A Treatise on Crataegus. Cincinnati: Lloyd Brothers Pharmacists, Inc.
Lou Zhicen (ed.-in-chief). 1987. Colour Atlas of Chinese Traditional Drugs. Vol. 1. Beijing: Science Press.
Lu, H.C. 1986. Chinese System of Food Cures. NY: Sterling.
Madaus, G. 1938. Lehrback der Biologischen Heilmittel. New York: Georg Olms.
Meier, B. 1989. Plant vs. synthetic medicines. Schweiz. Apothek.-Zeit. 19: 472-477.
Middleton, E. 1988. Some biological properties of plant flavonoids. Annals of Allergy 61: 53-57.
Nikolov, N., et el. 1982 New flavonoid-glycosides from Crataegus monogyna and Crataegus pentagyna. Planta Med. 44: 50-3.
O'Connolly, M., et al. 1987. Treating older, multi-morbid patients with angina pectoris symptoms, a placebo-controlled crossover double-blind study with Crataegutt novo. Therapiewoche 37: 3587.
Occhiuto, F., et al. 1986. Study comparing the cardiovascular activity of shoots, leaves and flowers of C. laevigata L. II. Effect of extracts and pure isolated active principles on the isolated rabbit heart. Plantes Med. phytother. 20: 52-63.
Parkinson, J. 1640. Theatrum Botanicum: The Theater of Plants. London: Tho. Cotes.
Perry, L.M. 1980. Medicinal Plants of East and Southeast Asia: Attributed properties and uses. Cambridge: The MIT Press.
Pharmacopeia Committee of the Ministry of Health. 1985. Pharmacopeia of the People's Republic of China (Zhong Hue Ren Min Gong He Guo Yao Dian, Ti Bu). Part 1. Beijing: People's Health Publishing House and Chemical Industry Publishing House.
Pickering, C. 1879. Chronological History of Plants. 2 vols. Boston: Little, Brown and Co.
Rafinesque, C.S. 1830. Medical Flora or Manual of the Medical Botany of the United States. Vol. 2. Philadelphia: Samuel C. Atkinson.
Sajner, J. & O. Veris. 1963. Histamine-effect from hawthorn infusion. Arzneim.-Forsch. 13: 52-4.
Sargent, C.S. 1933. Manual of the Trees of North America. 2nd. ed. Boston: Houghton Mifflin Company.
Schimmer, O., et el. 1988. The mutagenic potencies of plant extracts containing quercetin in Salmonella typhirmurium TA98 and TA100. Mutat. Res. 206: 201-8.
Smith, F.P. & G.A. Smart. 1973. Chinese Medicinal Herbs. San Francisco: Georgetown Press.
Steinman, et al. 1984. Immediate-type hypersensitivity to Crataegus monogyna (hawthorn). Contact Dermatitis 11: 321.
Syme, J.T.B. & J.E. Sowerby. 1863-1886. English Botany, 12 vols. & supplement. London: Robert Hardwicke.
Tucker, A.O., J.A. Duke & S. Foster. 1990. Tucker, A.O. 1990. Botanical Nomenclature of Medicinal Plants. In L.E. Craker and J.E. Simon, eds. Herbs, Spices, and Medicinal Plants: Recent Advances in Botany, Horticulture, and Pharmacology. Vol. IV. Phoenix, AZ: Oryx Press. In press.
Wagner, H., et al. 1984. Plant Drug Analysis. New York: Springer-Verlag.
Yanovsky, E. 193., Food Plants of the North American Indians. USDA Misc. Pub. No. 237.
Zeylstra, H. 1983. Crataegus. New Herbal Practitioner 9: 53-61.
Zohary, D. & M. Hopf. 1988. Domestication of Plants in the Old World. New York: The Clarendon Press, Oxford University Press.
Supplementary References (not cited in text)
Bercker, R. 1984. Myocardial insufficiency therapy of non-glycoside-requiring patients. Med. Welt. 35: 1567-9.
Bredneva, N.D. & I.A. Muravyov. Development of new methods for production of a Hawthorn tincture. Farmatsiya 36: 33-7. (Russian).
Ficarra, P. et el. 1984b. Analysis of 2-phenyl-chromone derivatives and chlorogenic acid. Il Farmaco-Ed. Pr. 39: 342-354.
Geissberger, W. & R.L. Galeazzi. 1977. Personal research on dosage of plant glycosides. Schweiz Mea. Wochenschr. 107: 887-9. (Human study, German).
Godfrey, R.K. 1988. Trees, Shrubs, and Woody Vines of Northern Florida and Adjacent Georgia and Alabama. Athens: The University of Georgia Press.
Grigoreseu, Em., et el. 1985. Aspects in the determination of the extraction yield for obtaining Crataegus fluid extract. Farmacia (Bucharest) 33:129-34.
Hamon, N.W. 1988. Herbal medicine: Hawthorns (Genus Crataegus). Can. Pharm. J. 121: 708-9; 724.
Hiermann, A., et el. 1986. A method for the quantitative determination of procyanidins in Crataegus. Sci. Pharm. 54: 331-7. (German).
Kartez, J.T. and Rosmarie Kartez. 1980. A Synonymized Checklist of the Vascular Flora of the United States, Canada, and Greenland. Chapel Hill: University of North Carolina Press
Kartnig, Th., et al. 1987. Investigations on the procyanidin and flavonoid contents of Crataegus monogyna drugs. Sci. Pharm. 55: 95-100. (German).
Kaverina, N.V., et al. 1988. Study of specific antiarrhythmic activity displayed by drugs from Crataegus. Farmatsiya 37: 33-6. (Russian).
Kery, A., et al. 1977. Comparative study of flavonoids from C. laevigata L. and C. monogyna Jacq. Acta Pharm. Hung. 47:11-23. (Analysis, summary in English).
Kiseleva, T.L. & I.A. Samylina. 1988. Standardization of raw haws (Crataegus fructum). Farmatsiya 37: 19-21. (Russian).
Kiseleva, T. L., et el. 1989. Amino acid composition of the flowers of pharmacopoeial and nonpharmacopoeial species of Crataegus L. Rastitel'nye Resursy 25: 145-54.
Mabberly, D.J. 1987. The Plant Book: A Portable Dictionary of Higher Plants. New York: Oxford University Press.
Murakami, T. & Y. Lizuka. 1984. Effect of haw extract of hawthorn (C. cuneata) on blood pressure in SHRSP. Med. J. Kinsi. Univ. 9/4 Suppl.: 57-60.
Muth, H.W. 1976. Indications for treatment with Crataegus. Ther. Ggw. 115: 242-55. (Human, therapy, combination with digitalis, German).
Oswiecimska, M., et el. 1986. Proanthocyanidins in inflorescentia Crataegi (hawthorn inflorescence). Part I. Analysis of the commercial drug. Farm. Pol. 42:116-9.
Pasquale, A. de. 1986. Study comparing the cardiovascular activity of young shoots, leaves, and flowers of IL. I. Electrical activity and arterial pressure in the rat. Plantes Med. et Phytother. 20:37-51.
Petrov, L., et el. 1974. Studies on the vasoactive effect of the Cratemon preparation. Acta Physiol. Pharmacol. Bulg. 2: 82-9. (Animal, pharmacodynamics, English).
Rabasco, A. M., et al. 1984. High-performance chromatography of flavonoids in C. laevigata L. I. Reversed-phase high-pressure liquid chromatography. Farmaco 39: 158-69.
Sakai, K., et al. 1989. Effect of water extracts of aloe and some herbs in decreasing blood ethanol concentrations in rats. Chem. Pharm. Bull. 37: 155-9.
Sibiga, A., et al. 1986. Proanthocyanidins in inflorescentia Crataegi (hawthorn inflorescence). Part II. Determination of cyanidin chloride in galenic preparations. Farm. Pol. 42: 153-5.
Totte, J. & A.J. Vlietinck. 1986. Phytotherapy and cardio-vascular system. J. Pharm. Belg. 41: 330-61. (French).
Trunzler, G. 1980. Heart and circulatory activity in plant pharmacology. Ärztl Praxis 32: 950-6.
Trunzler, G. 1987. Cardioactive plants. Z. Phytother. 8:11-3. (German).
Weiss, R. F. 1988. Herbal Medicine. Stuttgart: Hippokrates Verlag GmbH. Reprinted in English by Beaconsfield, England: Beaconsfield Publishers, LTD.
Article copyright American Botanical Council.
~~~~~~~~
By Steven Foster and Christopher Hobbs
Table 3. The Major Consitutents and Activity of Crataegus spp.
((*) C. laevigata unless specified otherwise)
Constituent group & Constituent Activity (If Known)
Aromatic Carboxylic acids
not studied in Crataegus
(phenolic derivatives)
chlorogenic, caffeic acids (1)
(1,2,3)
Sterols
not studied in Crataegus
beta-sitosterol (1) 0.51-0.62 ,
(fl) 0.65-0.78 (4,4)
Pentacyclic Triterpenes
no effect (5,6); - chronotropic, +
oleanolic acid, ursolic acid, inotropic, and coronary dilation
effects
acantolic acid, neotegolic acid, (7); antiarrhythmic (8)
2-alpha-hydroxy-oleanic acid
(syn. crataelogic acid) (l,f)
(total in leaves,0.5-1.4%; fruit
0.3-1.4%; blossoms, 0.7-1.2%)
(3,9,10,11)
Flavonoids:
Flavones (3,12,13,14,15)
mixture of flavones orally in mice show
hyperoside (hyperin) (1)
weak sedative CNS effect (in dose = to
11
vitexin (1)
gms in a 135 lb rat), humans more
vitexin-rhamnoside (1)
sensitive to sedatives (16); hyperoside
vitexin-4'-L-rhamnoside(main one) iv to dogs lowered blood pressure prob.
vitexin-4'-L-rhamno-d-glucoside from peripheral vasodilat., no effect
on
vitexin-4'-7-di-d-glucoside
heart (17);
rutin
quercetin-3-rhamno-galactoside
2.2% total flavonoid standardized oral dose in rats w/ placebo group
extract (according to the 9th strongly potentiated protective effects
German Pharmacopeia -- DAB 9) of garlic against isoprenaline-induced
heart damage (18)
(*) Crataegus monogyna
See Crataemon section
total flavonoid content 1.8% (19)
or 4.4%, 0.64% hyperoside (20)
vitexin-4'-O-rhamnosi(deacylated)
(main constituent) (21);
vicenins-1,2,3; schaftoside;
iso-, neo- and neoiso-schaftoside
(22); quercetin, crateside,
luteolin-7-O-glycoside, orientin,
iso-orientin (Nikolov, et al.,
1982) Catechins
(6)
(+)-catechin (11)
(-)-epicatechin (23,24,25)
(*) heptahydroxyflavan glycoside iv, ia: increase in circulation,
(26) from "Eurhyton" (a
(27); iv in cats: hypotensive, +
polycondensation product of inotropic (28)
flavan units)
"flavan polymer fraction"
Proanthocyanidins (syn.
procyanidins, pycnogenol)
pycnogenol from pine-needle extract is
flavan dimers, hexamers,
sold on the American health food market
oligomers,polymers;total,1-3�9) as an oxygen radical scavenger
oligomeric proanthocyanidins (30) (anti-oxidant) (author's observation);
cardioactive in vitro (7)
cats, mice, iv, ip: lowers blood
pressure & body temp., CNS sedative
(31,32)
oligomeric procyanidin
long-term oral dose in dogs led to up
70%
(standardized -- (OPC)
increase in blood flow in left
ventricle (33)
polymers of proanthocyanidins showed broad spectrum of antibiotic
(condensed tannins)
properties (34)
Commercial preparations
(*) Esbericard (water extr.
iv, ia in dogs: vasodilation peripheral
of flowers and leaves +(flowers?) resistance lowered (35, 36, 37)
(1:3)standardized to 8�ondensed uncontrolled study with 40 older heart
flavans 1-catechin part of total patients showed clinical improvement,
activity
even when previously digitialized (38)
(*)Crataegutt(EtOH extract of fl, guinea pig heart in vitro: increase in
1 of C. monogyna + C. laevigata, blood flow, potentiated pos. inotropic
standardized to 200 mg
effects of digitalis, etc. (39); oral
procyanidins/100 ml)
administration in dogs led to increase
in blood flow to left ventricle of heart (40); oral administration in rabbits significantly reduced anoxic-induced recovery time of heart muscle + refs. (41); oral dose in dogs
led to 25-39% increase (42); oral dose vs. placebo in 36 humans w/decreased
heart performance benefited heart and subjective improvement (43); controlled d-blind study w/oral application showed increased coronary perfusion and economizing of myocardial oxygen consumption, normalization of ECG; treatment suitable for NYHA stages I and II not yet needing nitrates, beta-receptor blocking agents and Ca antagonists (44) (*) Crataemon (total flavonoid in small amounts, reduces oxygen mixture from C. monogyna (flowers consumption,activating respiration in and leaves) contains 19 heart mitochondria in vitro, possibly
flavonoids:(47) due to a zinc-flavonoid complex (45); iv dose in dogs raises coronary blood flow (46)[contains alcohol?];1 oral administration in rats in a controlled study led to increased vascularization in heart after induced infarction quercetin, kaempferol, hyperoside, crataeside, glogoside, rutin, spiraeoside, quercetin-3-O-rhamno-galactoside, luteolin-7-O-glucoside+ 12 flavone C-glycosides (vitexin,
isovitexin,orientin, isoorientin, monoacetyl-isoorientin, rhamnosyl-vitexin, 2 C-glycosides of apigenin and others (l,fl) (28,29) Purine (xanthine) derivatives no data
adenosine, adenine, guanine, uric acid (1) (3,11,48) Saponins (total fraction) from no data C. pentagyna (49) Amines (3) ethylamine, dimethylamine,
show + inotropic effect in
vitrotrimethylamine,isobutylamine (guinea pig papillary muscle) (50)
isobutylamine,
isoamylamine, ethanolamine,
beta-phenylethylamine, choline,
acetylcholine (1) phenethylamine,
o-methoxyphenethylamine, tyramine
(fl) polyamines(spermindine)(11)
Amino Acids (51)
Total free AA:leaves(22.8 mmol/kg flowers considered to be a good
dry weight), flowers (52.3),
source of cardioactive compounds (52)
fruits (6.3)
Misc. (3,11)
Vitamin C (1 = 0.18%, 0.14-0.25% no data
in C. rnonogyna)
Essential oil (1) 0.157%
--
Sorbitol
--
Amygdalin (1=0.15%)
--
Pectin
--
Aesculin (in the bark)
--
Mineral salts, especially sodium --
Whole plant extract
pos. inotropic -- guinea pig heart
Water decoction
muscle (53); iv in rats showed
dose-dependant hypotensive effect
(54)
Extracts of Crataegus pinnatifida among 4 plants tested, induced
greatest SOD activity in red blood
cells in vitro (55)
Hawthorn in Chinese Medicine
C. pinnatifida Bge. var.
show cardiotonic activity in animals
major N.E..Br.,C. pinnatifidaBge. in vitro and in vivo; in humans
or C. cuneata Sieb. et Zucc.
(all studies uncontrolled) extracts lowered serum cholesterol, relieved symptoms of angina, hypertension, palpitations, insomnia, coronary insufficiency, dyspepsia, successfully treated bacillary dysentery and enteriris, hepatitis,and pyelonephritis (56)
Footenootes - Table 3
(1.) Hockerts, T. & G. Mülke. 1955. Studies on the coronary effect of aqueous extracts of Crataegus. Arzneim.-Forsch. 5: 755-7.
(2.) Ficarra, P., et el. 1984a. High-performance liquid chromatography of flavonoids in C. laevigata L. I:reversed-phase high pressure liquid chromatography. Il Farmaco-Ed. Pr. 39: 148-57.
(3.) List & Hörhammer, opus cited.
(4.) Bersin, T. &A. MÜller. 1952. Concerning the constituents of Crataegus oxyacantha. II: betasitosterin and oleanic acid. Helv. Chim. Acta 35: 1891-1895.
(5.) Dörner, J. & H.J. Kuschke. 1955. Do Crataegus triterpenic acids (Crataogus acids) possess a pharmacodynamic effect? Archiv fÜr exper. Pathologie and Pharmacologie 225:144.
(6.) Nikolov, et al. (1981), opus cited.
(7.) Occhiuto, F., et al. 1986. Study comparing the cardiovascular activity of shoots, leaves and flowers of C. laevigata L. II: Effect of extracts and pure isolated active principles on the isolated rabbit heart. Plantes Mtd. Phytother. 20: 52-63.
(8.) Occhiuto, F., et al. 1986. Study comparing the cardiovascular activity of young shoots,leaves and flowers of C. laevigata L. I: Electrical activity and arterial pressure in the rat. Plantes Med. Phytother. 20: 37-51.
(9.) Bersin, T. & MÜller. 1951. Concerning the constituents of Crataegus oxyacantha L. I: ursolic acid. Helv. Chim. Acta 34: 1868-72.
(10.) Braasch & Bienroth, opus cited.
(11.) Steinegger & Hänsel, opus cited.
(12.) Ficarra, et al. (1984a), opus cited.
(13.) Fisel, J. 1965. New flavonoids from Crataegus. I: Isolation of an acetylated vitexin-4'rhamnoside from C. monogyna L. Arzneim.-Forsch. 15: 1417-21.
(14.) Fisel, J. 1966. New flavonoids from Crataegus. II: Isolation of a mixture of rutin and quercetin-3-rhamnoglactoside from C. monogyna L. (xx CH journal name coming).
(15.) Kowalewski, Z. & K. Mrugasiewicz. 1968. New flavanonheterosides in C. phenophyrum. Planta Med. 19:311-17.
(16.) Loggia, R.D., et el. 1983. Depressive effect of C. laevigata L. on central nervous system in mice. Sci. Pharm. 51: 319-24. (English).
(17.) Lievre, M., et al. 1985. Assessment in the anesthetized dog of the cardiovascular effects of a pure extract (hyperoside) from hawthorn. Ann. Pharm. Fran. 43:471-7.
(18.) Ciplea, A.G. & K.-D. Richter. 1988. The protective effect of Allium sativum and Crataegus on isoprenaline-induced tissue necroses in rats. Arzneim.-Forsch. 38: 1583-92. (English).
(19.) Nikolov, N. & V. Ivanov. 1969. Flavonoid composition of C. monogyna. I:Isolation of a flavonoid mixture from the leaves. Farmatsiya 19: 32-7. (Chem. Ab. 73: 32285v).
(20.) Simova, M. & T. Pangarova. 1983. Flavonoid determination in hawthorn. Pharmazie 38: 791-2.
(21.) Pietea, P., et al. 1986. Isocratic liquid chromatographic method for the simultaneous determination of Passiflora incarnata L. and C. monogyna flavonoids in drugs. J. of Chrom. 357: 233-8.
(22.) Nikolov, N., et al. 198 lb. Di-C-glycosylflavones from C. monogyna. Phytochem. 20: 2780-1.
(23.) Rewerski, W. & S. Lewak. 1967. Some pharmacological properties of flavanpolymers from hawthorn (C. Laevigata). Arzneim.-Forsch. 17: 490.
(24.) Rewerski, W., et al. 1971. Some pharmacological properties of oligomeric procyanidins isolated from hawthorn (C. Laevigata). Arzneim.-Forsch. 21: 886-7.
(25.) Schwabe, W. & R. Neu. 1960. Pharmacological examination of a substance from Crataegus. Arzneim.-Forsch. 10: 60.
(26.) Bersin, T. 1955. Studies on the ingredients of Crataegus oxycantha L. Arzneim.-Forsch. 5:490.
(27.) Engelking, R. & F. Willig. 1958. The cardiac and circulatory action of a water-soluble Crataegus ingredient (heptahydroxyflavanglycoside) in dogs. Arzneim.-Forsch. 8: 39-42.
(28.) Rewerski, W. & Lewak, S. 1967. Some pharmacological properties of flavan polymers isolated from hawthorn (C. laevigata). Arzneim.-Forsch. 17: 490-1.
(29.) Steinegger, E. & R. Hänsel. 1988. Handbook of Pharmacognosy and Phytopharmacy. New York: Springer-Verlag. (German).
(30.) Hö1zl, J. & A. Strauch. 1977. Investigation on the biosynthesis of oligomer procyanidins of Crataegus. Planta Med. 32: 141-53.
(31.) Reweeski, W., et al. Some pharmacological properties of oligomeric procyanidin isolated from hawthorn (C. laevigata). Arzneim.-Forsch. 21: 886-8.
(32.) Rewerski, et al. (1971), opus cited.
(33.) Roddewig, C. & H. Hensel. 1977. Reaction of local myocardial blood flow in non-anesthetized dogs and anesthetized cats to oral and parenteral application of a Crataegus fraction (oligomere procyanidins). Arzneim.-Forsch. 27: 1407-10.
(34.) Porter, L.J. 1986. Proanthocyanidin polymers (PAP) have broad-spectrum antibiotic properties. Aust. J. Chem. 39: 557-62.
(35.) Kovach, A.G.B., et al. Effects of an extract obtained from C. laevigata on coronary blood flow in dogs. Arzneim.-Forsch. 9: 378-9.
(36.) Schwabe, W. & R. Neu. Pharmacological investigations of a new substance isolated from Crataegus. Arzneim.-Forsch. 10: 60-1.
(37.) Ammon & Händel (1981c).
(38.) Berker, R. 1984. Therapy in heart insufficiency where glycosides are not required. Medwelt 35: 1567-9.
(39.) Trunzler, G. & E. Schuler. Comparative studies on the effects of a Crataegus extract, digitoxin, digoxin and g-strophanthin in the isolated heart of homoiothermals. Arzneim.-Forsch. 12: 198-202.
(40.) Mäves, W.H. & H. Hensel. 1974. Changes in local myocardial blood flow following oral administration of a Crataegus extract to non-anesthetized dogs. Arzneim.-Forsch. 24: 7835.
(41.) Kanno, T., et al. 1976. Reduction of the hypoxia-induced depression in the intracellular electrical activity of the ventricular muscle fibers of the rabbit fed on food containing Crataegutt. Jap. Heart J. 17: 512-520.
(42.) Mävers, W.H. & H. Hensel. 1974. Changes in local blood flow after oral application of a Crataegus extract in un-narcotised dogs. Arzneim.-Forsch. 24: 783.
(43) O'Connolly, M., et al. Treatment of decreasing cardiac performance (NYHA stages I to II) in advanced age with standardized Crataegus extract. Fortschr. Med 104: 805-8.
(44.) Hanak, Th. & M.H. Bruckel. 1983. Treatment of mild stable forms of angina pectoris with a standardized Crataegus extract. Therapiewoche 33/34: 4331-3.
(45.) Ivancheva, E., et al. 1976. Effect of Crataemon on the respiration of isolated mitochondria. Acta Phys. Pharm. Bulg. 2: 35-40.
(46.) Taskov, M. 1977. On the coronary and cardiotonic action of Crataemon. Acta Phys. Pharm. Bulg. 3: 53-57. (English).
(47.) Guendjev, Z. 1977. Experimental myocardial infarction of the rat and stimulation of the revascularization by the flavonoid drug Crataemon. Arzneim.-Forsch. 27:1576-9. (English).
(48.) Kranen-Fiedler, U. 1955. Ingredients obtained from Crataegus. Arzneim.-Forsch. 5: 757-8.
(49.) Gusseinow, D.J. 1965. On the pharmacology of the total saponins from C. pentagyna W. et K. Farmakol. i Toksikol. 28: 172.
(50.) Wagner, H. & J. Grevel. 1982. Cardioactive drugs IV: Cardiotonic amines from C. Oxyacantha. Planta Med. 45: 98-101.
(51.) Kiseleva, T.L., et al. 1989. Amino acid composition of the flowers of pharmacopoeial and non-pharmacopoeial species of Crataegus L. Rastitel'nye Resursy 25: 145-54.
(52.) Kiseleva, T.L., et al. The free amino acid composition in different organs of C. oxyacantha (Poir.) DC. 1989. Rastitel'nye Resursy 25: 92-7.
(53.) Vogel, G. 1975. Predictability of the activity of drug combinations -- yes or no? Arzneim.Forsch. 25: 1356-65.
(54.) Abdul-Ghani, A.-S., et el. 1987. Hypotensive effect of C. oxyacantha. Int. J. Crude Drug Res. 25: 216-20.
(55.) Dai, Y.R., et al. 1987. Effect of extracts of some medicinal plants on superoxide dismutase activity in mice. Planta Med. 53: 309-10.
(56.) Chang, H.-M. & P. P-H. But. 1986. Pharmacology and Applications of Chinese Materia Medica, 2 vols. Philadelphia: World Scientific.
References
Alcock, R.H. 1876. Botanical Names for English Readers. London: L. Reeve & Co.
Alleyne, J. 1733. The New English Dispensatory. London: Tho. Astley.
Ammon, H.P.T. & M. Händel. 1981a. Crataegus, toxicology and pharmacology. Part I. toxicology. Planta Med. 43: 105-120.
Ammon, H.P.T. & M. Händel. 1981b. Crataegus, toxicology and pharmacology. Part II: pharmacodynamics. Planta Med. 43:313-322 (with references).
Ammon, H.P.T. & M. Händel. 1981c. Crataegus, toxicology and pharmacology. Part III: pharmacodynamics and pharmacokinetics. Plante Med. 43: 209-239.
Anon. 1927. Facsimile Reproductions of the Principal Labels of Specific Medicines. Cincinnati: Lloyd Brothers Pharmacists, Inc.
Bailey, L.H. 1939. The Standard Cyclopedia of Horticulture. Vol. 1. New York: The Macmillan Company.
Bensky, D. & A. Gamble. 1986. Chinese Herbal Medicine: Materia Medica. Seattle: Eastland Press.
Braasch, W. & W. Bienroth. 1960. Peripheral circulatory effects of an aqueous extract from Crataegus in dogs. Arzneim.-Forsch. 10: 127-9.
Chekalinskaya, I.I., et al. 1985. Chemosystematic study of plants of the genus Crataegus. Referativnyi Zhurnal 9V548.
Cockayne, O. (ed.). 1864-6. Leechdoms, Wortcunning, and Starcraft of Early England. London:
Costa, R., et al. 1986. Comparative study of the cardiovascular activity of young shoots, leaves and flowers of C. laevigata L. Part III. Protective action on the isolated rat heart against arrhythmogenic agents and arrhythmias induced by reperfusion. Plantes Med. Phytother. 20: 115-28.
Dirr, M.A. and C.W. Heuser, Jr. 1987. The Reference Manual of Woody Plant Propagation: From Seed to Tissue Culture. Athens, Georgia: Varsity Press, Inc.
Duncan, W.H. and M.B. Duncan. 1988. Trees of the Southeastern United States. Athens: University of Georgia Press.
Eggleston, W.W. 1908. The Crataegi of the Northeastern United States and Adjacent Canada. Rhodora 10 (113): 73-84.
Emerson, G.B. 1875. A Report on the Trees and Shrubs of Massachusetts. 2nd ed. Boston: Little Brown and Company.
Erichsen-Brown, C. 1979. Use of Plants for the Past 500 Years. reprint ed. 1989; Medicinal and other uses of North American Plants. New York: Dover Publication.
Everett, Thomas H. 1981. The New York Botanical Garden Illustrated Encyclopedia of Horticulture. Vol. 3. New York: Garland Publishing, Inc.
Flück, H. & H. Schwabe. 1968a. Investigation of herb conservation with C. monogyna in the temperature range 20-100 deg. C. Part I: Quantitative Measurements of flavon heterosides. Planta Med. 16: 257-68.
Flück, H. & H. Schwabe. 1968b. Investigation of herb conservation with C. monogyna in the temperature range 20-100 deg. C. Part II: Enzymatic Decomposition of Flavon Heterosides. Planta Med. 16: 377-87.
Frisk, G. 1949. A Middle English Translation of Macer Floridus de Viribus Herbarum. Cambridge: Harvard University Press.
Gerard, J. 1597. The Herbal or Generall Historie of Plantes....London: John Norton.
Gerard, J. 1633. The Herbal or General Historie of Plants....Revised and enlarged by T. Johnson, reprinted by Dover Publications, New York. 1975.
Gunther, R.T. 1933. The Greek Herbal of Dioscorides. Hafner Publishing Co. 1968.
Hahn, F., et al. 1960. Preparation and pharmacological investigation of a new therapeutic agent obtained from Crataegus oxyacantha. Arzneim-Forsch. 10:825.
Hanak, Th. 1983. Treatment of mild stable forms of angina pectoris with a standardized Crataegus extract. Therapiewoche 33/34: 4331-3.
Herbarium Apulei. 1481. Milano: Edizioni il Polifilo (1979).
Hooper, D. 1929. On Chinese medicine: drugs of Chinese pharmacies in Malaya. The Gardens' Bulletin 6:1-165.
Hort, A.F. 1948. Theophrastus Enquiry into Plants. Cambridge: Harvard University Press.
Hou, J.P. 1977. The Development of Chinese Herbal Medicine and the Pen-ts'ao. Comparative Medicine East and West 5 (2): 117-122.
Hsu, H.-Y., et el. 1986. Oriental Materia Medica. Long Beach: Oriental Healing Arts Institute.
Hsu, H.Y. et al. 1986. Oriental Materia Medica: A Concise Guide. Long Beach, CA: Oriental Healing Arts Institute.
Institutum Botanicum Pekinense Academiae Sinicae. 1974. Flora Reipublicae Popularis Sinicae Vol. 36. Rosaceae(1) (Chinese).
Iwamoto, M, et al. 1981. Clinical effect of Crataegutt in ischaemic heart disease and/or hypertensive origin. Planta Meal. 42: 1.
Jones, W.H.S. 1953. Pliny Natural History (23-79 AD). Cambridge: Harvard University Press.
Levey, M. & N. Al-Khaledy. 1967. The Medical Formulary of Al-Samarqandi. Philadelphia: University of Pennsylvania Press.
Liberty Hyde Bailey Hortorium, Staff of the. 1976. Hortus Third. NY: Macmillan, 1290 pp.
List, P.H. & L. Hörhammer. 1969-79. HagersHandbuch der Pharrnazeutischen Praxis, vols. 2-6a,b,c. New York: Springer-Verlag.
Little, E.L. 1980. The Audubon Society Field Guide to North American Trees. New York: Alfred A. Knopf.
Lloyd, J.U. 1917. A Treatise on Crataegus. Cincinnati: Lloyd Brothers Pharmacists, Inc.
Lou Zhicen (ed.-in-chief). 1987. Colour Atlas of Chinese Traditional Drugs. Vol. 1. Beijing: Science Press.
Lu, H.C. 1986. Chinese System of Food Cures. NY: Sterling.
Madaus, G. 1938. Lehrback der Biologischen Heilmittel. New York: Georg Olms.
Meier, B. 1989. Plant vs. synthetic medicines. Schweiz. Apothek.-Zeit. 19: 472-477.
Middleton, E. 1988. Some biological properties of plant flavonoids. Annals of Allergy 61: 53-57.
Nikolov, N., et el. 1982 New flavonoid-glycosides from Crataegus monogyna and Crataegus pentagyna. Planta Med. 44: 50-3.
O'Connolly, M., et al. 1987. Treating older, multi-morbid patients with angina pectoris symptoms, a placebo-controlled crossover double-blind study with Crataegutt novo. Therapiewoche 37: 3587.
Occhiuto, F., et al. 1986. Study comparing the cardiovascular activity of shoots, leaves and flowers of C. laevigata L. II. Effect of extracts and pure isolated active principles on the isolated rabbit heart. Plantes Med. phytother. 20: 52-63.
Parkinson, J. 1640. Theatrum Botanicum: The Theater of Plants. London: Tho. Cotes.
Perry, L.M. 1980. Medicinal Plants of East and Southeast Asia: Attributed properties and uses. Cambridge: The MIT Press.
Pharmacopeia Committee of the Ministry of Health. 1985. Pharmacopeia of the People's Republic of China (Zhong Hue Ren Min Gong He Guo Yao Dian, Ti Bu). Part 1. Beijing: People's Health Publishing House and Chemical Industry Publishing House.
Pickering, C. 1879. Chronological History of Plants. 2 vols. Boston: Little, Brown and Co.
Rafinesque, C.S. 1830. Medical Flora or Manual of the Medical Botany of the United States. Vol. 2. Philadelphia: Samuel C. Atkinson.
Sajner, J. & O. Veris. 1963. Histamine-effect from hawthorn infusion. Arzneim.-Forsch. 13: 52-4.
Sargent, C.S. 1933. Manual of the Trees of North America. 2nd. ed. Boston: Houghton Mifflin Company.
Schimmer, O., et el. 1988. The mutagenic potencies of plant extracts containing quercetin in Salmonella typhirmurium TA98 and TA100. Mutat. Res. 206: 201-8.
Smith, F.P. & G.A. Smart. 1973. Chinese Medicinal Herbs. San Francisco: Georgetown Press.
Steinman, et al. 1984. Immediate-type hypersensitivity to Crataegus monogyna (hawthorn). Contact Dermatitis 11: 321.
Syme, J.T.B. & J.E. Sowerby. 1863-1886. English Botany, 12 vols. & supplement. London: Robert Hardwicke.
Tucker, A.O., J.A. Duke & S. Foster. 1990. Tucker, A.O. 1990. Botanical Nomenclature of Medicinal Plants. In L.E. Craker and J.E. Simon, eds. Herbs, Spices, and Medicinal Plants: Recent Advances in Botany, Horticulture, and Pharmacology. Vol. IV. Phoenix, AZ: Oryx Press. In press.
Wagner, H., et al. 1984. Plant Drug Analysis. New York: Springer-Verlag.
Yanovsky, E. 193., Food Plants of the North American Indians. USDA Misc. Pub. No. 237.
Zeylstra, H. 1983. Crataegus. New Herbal Practitioner 9: 53-61.
Zohary, D. & M. Hopf. 1988. Domestication of Plants in the Old World. New York: The Clarendon Press, Oxford University Press.
Supplementary References (not cited in text)
Bercker, R. 1984. Myocardial insufficiency therapy of non-glycoside-requiring patients. Med. Welt. 35: 1567-9.
Bredneva, N.D. & I.A. Muravyov. Development of new methods for production of a Hawthorn tincture. Farmatsiya 36: 33-7. (Russian).
Ficarra, P. et el. 1984b. Analysis of 2-phenyl-chromone derivatives and chlorogenic acid. Il Farmaco-Ed. Pr. 39: 342-354.
Geissberger, W. & R.L. Galeazzi. 1977. Personal research on dosage of plant glycosides. Schweiz Mea. Wochenschr. 107: 887-9. (Human study, German).
Godfrey, R.K. 1988. Trees, Shrubs, and Woody Vines of Northern Florida and Adjacent Georgia and Alabama. Athens: The University of Georgia Press.
Grigoreseu, Em., et el. 1985. Aspects in the determination of the extraction yield for obtaining Crataegus fluid extract. Farmacia (Bucharest) 33:129-34.
Hamon, N.W. 1988. Herbal medicine: Hawthorns (Genus Crataegus). Can. Pharm. J. 121: 708-9; 724.
Hiermann, A., et el. 1986. A method for the quantitative determination of procyanidins in Crataegus. Sci. Pharm. 54: 331-7. (German).
Kartez, J.T. and Rosmarie Kartez. 1980. A Synonymized Checklist of the Vascular Flora of the United States, Canada, and Greenland. Chapel Hill: University of North Carolina Press
Kartnig, Th., et al. 1987. Investigations on the procyanidin and flavonoid contents of Crataegus monogyna drugs. Sci. Pharm. 55: 95-100. (German).
Kaverina, N.V., et al. 1988. Study of specific antiarrhythmic activity displayed by drugs from Crataegus. Farmatsiya 37: 33-6. (Russian).
Kery, A., et al. 1977. Comparative study of flavonoids from C. laevigata L. and C. monogyna Jacq. Acta Pharm. Hung. 47:11-23. (Analysis, summary in English).
Kiseleva, T.L. & I.A. Samylina. 1988. Standardization of raw haws (Crataegus fructum). Farmatsiya 37: 19-21. (Russian).
Kiseleva, T. L., et el. 1989. Amino acid composition of the flowers of pharmacopoeial and nonpharmacopoeial species of Crataegus L. Rastitel'nye Resursy 25: 145-54.
Mabberly, D.J. 1987. The Plant Book: A Portable Dictionary of Higher Plants. New York: Oxford University Press.
Murakami, T. & Y. Lizuka. 1984. Effect of haw extract of hawthorn (C. cuneata) on blood pressure in SHRSP. Med. J. Kinsi. Univ. 9/4 Suppl.: 57-60.
Muth, H.W. 1976. Indications for treatment with Crataegus. Ther. Ggw. 115: 242-55. (Human, therapy, combination with digitalis, German).
Oswiecimska, M., et el. 1986. Proanthocyanidins in inflorescentia Crataegi (hawthorn inflorescence). Part I. Analysis of the commercial drug. Farm. Pol. 42:116-9.
Pasquale, A. de. 1986. Study comparing the cardiovascular activity of young shoots, leaves, and flowers of IL. I. Electrical activity and arterial pressure in the rat. Plantes Med. et Phytother. 20:37-51.
Petrov, L., et el. 1974. Studies on the vasoactive effect of the Cratemon preparation. Acta Physiol. Pharmacol. Bulg. 2: 82-9. (Animal, pharmacodynamics, English).
Rabasco, A. M., et al. 1984. High-performance chromatography of flavonoids in C. laevigata L. I. Reversed-phase high-pressure liquid chromatography. Farmaco 39: 158-69.
Sakai, K., et al. 1989. Effect of water extracts of aloe and some herbs in decreasing blood ethanol concentrations in rats. Chem. Pharm. Bull. 37: 155-9.
Sibiga, A., et al. 1986. Proanthocyanidins in inflorescentia Crataegi (hawthorn inflorescence). Part II. Determination of cyanidin chloride in galenic preparations. Farm. Pol. 42: 153-5.
Totte, J. & A.J. Vlietinck. 1986. Phytotherapy and cardio-vascular system. J. Pharm. Belg. 41: 330-61. (French).
Trunzler, G. 1980. Heart and circulatory activity in plant pharmacology. Ärztl Praxis 32: 950-6.
Trunzler, G. 1987. Cardioactive plants. Z. Phytother. 8:11-3. (German).
Weiss, R. F. 1988. Herbal Medicine. Stuttgart: Hippokrates Verlag GmbH. Reprinted in English by Beaconsfield, England: Beaconsfield Publishers, LTD.
Article copyright American Botanical Council.
~~~~~~~~
By Steven Foster and Christopher Hobbs
|