|
|
|
|
|
|
|
|
|
Issue: 83 Page: 36-45
Steps Towards Revival of Graeco-Arabic Medicine in the Middle East: A New Project
by Stephen Fulder, Omar Said
HerbalGram. 2009;83:36-45 American Botanical Council
By Stephen Fulder, PhD, and Omar Said, PhD Tucked away between plant nurseries and small family fields of olives and wheat near the Galilee village of Kafr Kanna* is a shaded greenhouse. This greenhouse contains a large collection of medicinal plants, with approximately 120 species.1 The building is surrounded by classrooms, offices, a laboratory, a permaculture herb garden, and animals important to local Arab village life. This site, termed Al-Maissam, is a project of the Galilee Society, the largest charity in Israel and Palestine devoted to improving the health and environment of the Arab/Palestinian population. 
Greenhouse at the Al-Maissam project of the Galilee Society
Photo ©2009 Omar Said
The medicinal plant project began in 1995 as the brainchild of this article’s authors, Omar Said, PhD, a pharmacologist and a leader in research on Arab herbal medicine in the region, and Stephen Fulder, PhD, an international herbal expert and author of many books on herbs, as well as pioneering Arab herbalist Khaled Khalil and others. The project was based on the fact that herbs are of interest and value to all communities, being resources that cross boundaries and transcend conflict. It was hoped that it would also help to preserve threatened species of medicinal plants and sustain Arab herbal medicine as a cultural and economic resource. This project has grown enormously and is now the source of an initiative to bring both the herbs and the rich knowledge of traditional Arabian medicine to the United States, Europe, and elsewhere throughout the world.
GRAECO-ARAB MEDICINE The herbal tradition of the Middle East is part of an ancient medical system that is still alive and well.2 The correct term for this medical system is Graeco-Arab medicine, sometimes also called Hippocratic-Arab medicine, acknowledging its roots mainly in the ancient Greek medicine of Dioscorides (ca 40 –90 CE) and Galen (ca 130-200 CE). It is still a major healthcare resource for millions in a large part of the world, stretching from Pakistan to Morocco, with many therapists (hakims) practicing in an informal manner alongside the conventional Western medical system. They are often the first choice for handling common daily-life health problems. Though it is a major and intact medical system with its own literature, therapeutic principles and theory, specific materia medica, and methods of diagnosis and treatment, not much is known about Arabic medicine in the West, nor is much effort made to bring its remedies into Western markets. This may be based on an assumption that Arabic materia medica, as a foundation of Western herbal medicine, has nothing much left to teach practitioners of modern herbal medicine. Such an assumption may not be valid. 
Olive Tree Olea europaea Photo ©2009 Stephen Fulder From the 8th to the 13th century, the Arab caliphates (successive kingdoms ruled by the caliph from Bhagdad) became the Western world’s great center of learning and discovery. During this era, the Greek and Roman texts and knowledge, as well as those of Ayurveda and other medical systems, were translated, incorporated, and hugely extended. Hospitals, libraries, and pharmacies were established. Chemistry was applied to the processing of medicines, and pharmacy became an independent discipline from medicine. The approach was rational, experimental, exploratory, Hippocratic, and open, without the obsessive control by religious clergy that restricted medicine in Europe at the time. Great physicians included Abu Bakr Muhammad ibn-Zakaria al-Razi (953-986 CE), known as Rhazes in the West and author of 237 books (over half of which were on medical subjects), and the Andalusian genius scholar El Zahrawi (Albucasis 930 – 1013 CE), who is considered one of the greatest physicians-surgeons of all times. His work At-Tassrif is a medical encyclopedia of 30 volumes. The most influential Arabic contributor to medicine was the Persian physician abu-Ali al-Husayn ibn-Sina, known in the West by the Latinized version of his name, Avicenna (980-1037 CE). Avicenna’s influence continues to the present time within traditional Arabic medicine. His 5-volume text, al-Qanun fil-Tibb (the Canon or the Law of Medicine), was used as the main medical text until the 17th century in Europe. Along with Galen’s works it dominated medical thinking. The Canon’s first 4 books were devoted to hygiene, medicine, diseases, surgery, pathology, and contagious diseases. The fifth book dealt with pharmacy and was the standard materia medica for centuries. Another well-known sage was the Spanish Jewish Talmudist and physician Moses ben Maimon (Maimonides, 1135-1204 CE). 
Common Caper Capparis spinosa, growing in the hills of the Western Galilee.
Photo ©2009 Simon Irgens The knowledge of herbal remedies in Arabic medicine was rational and vast. Pharmacy was developed as a separate discipline for the first time.3 Rhazes used animals in order to test the safety and efficacy of extracted active ingredients. The Ibn Baytar Pharmacopoeia contained 1200 natural drugs (including more than 250 medicinal plants considered completely new to the medicine of the time), which were formulated and prescribed after differential diagnosis and according to a range of theories. These included the restorative and cleansing effects of bitters; the heating, drying, cooling nature of remedies; elimination as a method for restoration of immunity; analysis of tastes; pattern of humors; etc. This sophistication can be illustrated by the use of herbs for pain relief at the time. Arab chemists such as Ibn Hayan, Al-Kindi and others, who were founders of chemical science, were able to prepare various kinds of anaesthetic extracts from local herbs such as opium poppy (Papaver somniferum, Papaveraceae), mandrake (Mandragora officinarum, Solanaceae), henbane (Hyoscyamus niger, Solanaceae), hemlock (Conium maculatum, Apiaceae), aconite (Aconitum napellus, Ranunculaceae), and cannabis/marijuana (Cannabis sativa, Cannabinaceae). They listed them in order of strength and duration of pain relief, and they further defined dosages and antidotes. Before initiating surgery at that time, the physicians dipped a sponge in the plant extract and put it at the nose of the patient for general anesthetization or on the site of the surgery for local anesthesia. They also created oral and rectal dosage forms and patches, pastes, or fillings to provide pain relief in dentistry.
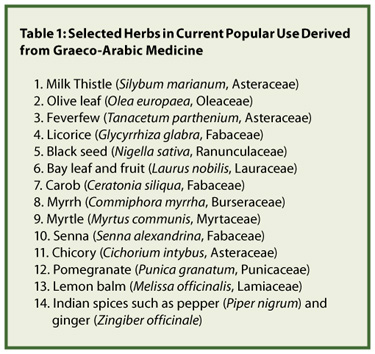
ARABIC FOUNDATION OF WESTERN HERBALISM It was only in the 10th century that the teachings of the Arab physicians, bringing with them Hippocrates (ca. 460–370 BCE), Galen, and the Greeks, began to slowly filter into Europe from the Arab world via the bridge of the Salerno School in Italy. Only in the 12th century, 400 years after pharmacy became a distinct profession in Persia, did it become so in Europe. At that time there was great enthusiasm in European apothecaries for the discovery of new remedies from the Arabs. Avicenna and Galen became the leading authorities guiding European medicine, and Arab herbal pharmacy was the source of European professional herbal therapeutics (described as ‘Galenical’ medicine). While pre-Arab European folk medicine continued, especially in the countryside, based on single local herbs simply prepared (‘simples’), the Galenical physicians and apothecaries found they could extend their professional territory (and fill their pockets) by prescribing and formulating exotic mixtures from Arabic medicine and giving them Latin names. Many new herbs were also introduced over time. A list of those that probably were introduced from Arabic medicine, based on information from various expert sources, is given in Table 1.
GREEK-ARABIAN MEDICINE TODAY There has been a decline in the great knowledge and use of herbs in the Arab world, mostly as a result of the increased availability of modern medicine. In some countries, such as Egypt, Syria, and Pakistan, traditional medicine is very strong and widely used. However, in certain areas, such as the Middle East, there is a real danger of much of indigenous Arab medicinal practices and knowledge disappearing altogether, further weakening traditional Arab culture and creating more insecurity, as well as forsaking a resource of inestimable economic and healthcare importance. In order to evaluate the current status of Arabic medicine and indigenous medicine in the Middle Eastern region, the authors of this article have carried out an ethnopharmacological survey of practitioners in Israel and Palestine, including the Bedouin in the desert regions.4 We were able to locate 31 therapists who regarded themselves as practitioners of Arabian herbal medicine. Among them, they used 150 plant species. The herbalists, on average aged 60, felt threatened and insecure. Very few passed on their knowledge to others or to the next generation on the grounds that it would be ‘stolen.’ Whereas practitioners were some of the most revered and educated members of the community in the past, this is evidently no longer the case today, particularly with the present dominance of modern medicine in the Middle Eastern region. Various ethnopharmacological surveys have shown that around 200 herbs are sold or traded in market places in the Middle Eastern region.5-8 A 2000 report by the Arab Union for Agriculture and Development has indicated that 23 plants are utilized in the medicinal products industry, 55 are used in perfume and cosmetics, 34 are involved in the food industry, and 10 species are used as botanical pesticides.9 A 2003 survey conducted in Jordan, where more than 100 herbalists were interviewed, revealed that there are around 150 plant remedies still in use as traditional substances.10 Preliminary data from the most recent and largest ethnobotanical survey in the region, which is still in process, shows that some 300 plant medicines, and quite a few animal and mineral remedies, are sold in traditional apothecaries (ittara stores). Some 400 herbs are in use within the Arab population of Israel and Palestine.11 A serious issue is that many herbs used in Arabic traditional medicine are now rare and that many have been eradicated from the Middle East for the usual reasons: ongoing destruction of their natural habitat, over-harvesting of wild species, and detrimental climatic and environmental changes. The hills, shoreline, and deserts of Israel and Palestine are extremely rich in plant diversity, with some 2700 species.12 Many of these are the progenitors of many important food crops of today, of which more than 700 are noted for their uses as medicinal plants used in Arabic traditional medicine.13 Some 30% of the flora are considered rare plants, and many of these are endangered.14 Some of these species, such as white wormwood (Artemisia herba alba, Asteraceae) and castor bean (Ricinus communis, Euphorbiaceae) are widely used throughout the Middle East and are also well known in European herbal medicine. Others, such as Judean wormwood (A. judaica) are used only locally. This was the background that encouraged the establishment of the Al-Maissam botanical garden. It is a place for collection and preservation of species, a location for research on agriculture and creation of herbal formulations, and above all, an educational project to revive interest in a great herbal medical system that was rapidly vanishing. Today, about 10,000 schoolchildren visit this site annually, mostly from the Israeli Arab community and some from the Jewish community. In addition, there is a laboratory where older children can make creams, concentrated and honey extracts, tinctures, soaps, and distilled oils in a way similar to the ancient apothecaries.
RESEARCH AND NEW PRODUCT DEVELOPMENT Part of the aim of the project was to create economic benefit for the Galilee Society charity, the team working on the project, and the Galilee Arab community. It was envisaged that a successful business would be an invaluable way of raising the profile and value of locally grown herbs as well as aid farmers, herbal experts, and all those involved in Arabic medicine. For this purpose the company Antaki Ltd was set up, taking its name from one of the last great scholars of Arabic medicine.15 (The blind Da’ud ibn Amar Al Antaki—‘David of Antioch’—was a renowned pharmacist, and his classic text Tadhkirah contains many plant remedies.) The company’s first task was to develop a library of tested formulations for common health problems, which would embody the full power of Greek-Arab medicine and its novel herbs. It was clear that many local remedies that are in use throughout the Middle East have never been properly researched, evaluated, or economically developed, and many of the tradition’s herbs are still new to Western countries. Moreover, we believed that many commercial herbal products have been developed by a process of formulation that has lacked knowledge and therapeutic logic. The main source of information for the creation of formulations is the vast written literature that still exists. Fortunately, as with Chinese and Indian medicine, the Arab physicians wrote everything down, and much of this material is in homes and in libraries throughout the Arab world. The literature is fascinating and intriguing, particularly since the herbal formulations are accompanied by a very clear description of differential diagnosis from which many health conditions widespread throughout the modern world can be precisely identified. For example, one useful ancient book is called The Nabatean Book of Agriculture.16 In it one finds not only remedies for human use but also a large number of veterinary prescriptions, plus methods of preparing botanical pesticides, fungicides, and crop treatments. However, literature alone is not enough, since there can be confusion regarding identification and names of plants. In addition, herbal medicine consists of a very large aggregate of overlapping information, which makes it difficult to define the primary remedies and combinations for each specific health problem. In our case, we sought additional confirmation and support in current use from the various published ethnopharmacological surveys,17,18 and our own, as well as from discussions with elders, healers, and practitioners, plus the accumulated knowledge of the founders of this project. In return, extensive education within Israel and Palestine was volunteered to restore credibility, legitimacy, and interest in the herbal tradition, and to benefit the whole community, including healers and clients. On the research front, potential candidates for herbal remedies have passed through an extensive screening process. Some basic screening tests were carried out on a very large number of plant extracts. Examples include in vitro toxicity testing by means of lactate dehydrogenase assays (LDH), screening for antioxidant activity, and toxicity studies in mice. These tests were carried out at the Galilee Society R&D Center, the Haifa Technion, and the Carmel Hospital, Haifa. A thorough review of published literature was carried out for each herb to confirm the kind of activity that was described in the Greek-Arabic literature. The literature search revealed many discrepancies, however. For example, Hypericum, the genus of St. John’s wort (H. perforatum, Clusiaceae), is well described as a very important remedy. It is called halawa by the local Arab population and dathi in the classical texts. Unlike the current accepted uses of Hypericum, in which anti-depressant effects take priority and antiseptic activities are regarded as minor, Greek-Arabic medicine recognizes its main use to be against burns and as an anti-inflammatory, anti-infective, and anti-parasitic herb, especially in skin treatment. It was also reported that it can be used to treat anxiety and menstrual problems. It is likely that more than one species in different areas are identified under the collective name of halawa (dathi). Being more indigenous to the Middle East region, the sources probably meant H. triquetrifolium, not H. perforatum. According to our high-performance liquid chromatography (HPLC) analyses of H. triquetrifolium, it contains less hypericin and more hyperforin than H. perforatum, and this may account for the differences in therapeutic emphasis.
Examples of Rationally Formulated Herbal Products: 1. Saltbush Formulations for Blood Sugar Problems and Metabolic Syndrome There are several well-known remedies for hyperglycemia, described in the Arab medical tradition as zihar, zaheer, zarab, diabeta, and diabatish. It was diagnosed by such symptoms as frequent urination, thirst, dry mouth, tiredness, etc. We identified the various herbs from traditional texts and then cross-checked them in published research literature and ethnobotany.19 One of the herbs mentioned was saltbush (Atriplex halimus, Chenopodiaceae). The Bedouin of the Negev desert pointed out the significant antidiabetic effect of this plant.20 We were pleasantly surprised to learn that researchers at the Ben-Gurion University in the Negev, Israel had already studied this plant some years earlier. It was a remarkable story centered around a small desert rodent called the sand rat (Psammomys obesus). This animal lives healthily in the wild, mostly on the leaves of the saltbush. As soon as it is given conventional rodent food or taken into a laboratory environment, it develops diabetes and metabolic syndrome (obesity, circulatory problems, etc.).21 Researchers found that this genetic tendency to diabetes and metabolic syndrome comes from a disturbed insulin system and insulin resistance, which also seems to be a key factor in the development of diabetes and metabolic syndrome in humans. The animal’s diabetes can be prevented and treated by giving it saltbush, saltbush extract, or even the ash from saltbush.22 Saltbush apparently helps the animal by restoring insulin sensitivity and reducing insulin resistance.23 A combination formula can be developed through the addition of further herbs to modify and slow sugar absorption from food to reduce cholesterol levels and to stimulate urination and removal of waste. For example, olive leaf (Olea europaea, Oleraceae) is added to reduce sugar levels, cholesterol, and fats through metabolic mechanisms. This proprietary combination has been tested pharmacologically and in a preliminary clinical observation study with promising results.24 Atriplex together with other herbs is therefore an herbal combination that is both scientifically and traditionally rational. 2. Zallouh in the Development of Sexual Potency Formulations
Another interesting example of a rationally studied herbal preparation is zallouh. Zallouh is the common name in the Middle East for the roots of the plant Ferula hermonis (Apiaceae), so named because it grows on the slopes of Mount Hermon in the Golan Heights. The plant grows in a relatively restricted area and is at risk of over-collection. It is also cultivated in certain countries such as Syria. It is botanically similar to F. communis, the giant fennel. There are several species of Ferula that grow locally and around the world, including the famous species F. asafetida, which is cultivated in Asia as a source of the spice resin asafetida. (The genus name Ferula comes from the Latin word for “walking stick,” because its stem was used as such. It is mentioned in the Bible [The Book of Job, Chapter 30, verse 2] in that context.) Zallouh has been used since ancient times as a mild tonic remedy and an aid to fertility and sexual energy. The Druze living in the Golan Heights, and also the local population of South Lebanon and Syria, appreciate the value of the roots especially in the elderly or in cases of impotence.3 Local people usually sell it mixed with honey. Some of the great scholars of traditional Arabic medicine (Ibn AlBeetar and Al-Antaki) suggested that zallouh is a sexual tonic and described the plant and the ecological range of F. hermonis.25 They called it Oud Alkerach Algabali (“stick from the mountains for the infirm,” or “walking stick”) and also Aaqer qarha (“fertility aid”). According to Dioscorides, this plant is used for the treatment of fatigue and impotence.† He also pointed out that the root or the resin of the cut stem can be used to clear the air passages and in cough or bronchial problems. Galen also mentions this plant. Preliminary research on this plant indicated that it may have a role in improving potency in sexual dysfunction. For example, sexually potent and impotent male rats were orally treated with extracts of F. hermonis. The acute administration stimulated libido in potent rats and improved copulatory performance in sluggish/impotent rats. However, chronic administration of the higher dose reduced testosterone and copulatory performance.26 There is similar evidence from researchers in Jordan that may show that higher doses of F. hermonis extracts, obtained using organic solvents and given over extended periods of time,27 have apparent adverse effects in rats and mice28 such as reduced fertility and sexual activity, which are opposite to the extracts’ desired effects. A product was formulated based on particular plant parts and extracts of the closely related F. asafetida, the spice plant. For women, extracts derived from Capparis spinosa (Capparaceae), the common caper, known in Arabic medicine for improving fertility in women, were also included. A relatively large number of Arab patients at fertility clinics in Israel have been administered these products as part of ongoing clinical research. Some of the male patients have had sperm counts and been motility tested before and after a 1-or 2-month course. The majority of patients with low sperm count (5-15 million/ml) showed a significant increase in sperm count during this period, with most also showing improvements in sperm motility, microstructure, and white blood cell count. Those with very low or zero sperm count sometimes showed a modest increase in sperm count, though it never reached normal levels.29 3. Topical Formulas for Skin Conditions
Dermatology is another area that was investigated because skin problems are widespread in the Arab community and because, according to Arabic medicine, herbs are very effective for these conditions. A partnership was established with the Dermatology Department of the Hebrew University under Professor Yoram Milner, supported by grants from the Israel Ministry of Infrastructure and private investors under the Technological Incubator process.
(a)Psoriasis: In searching for potential topical remedies for psoriasis, we tested the ability of low doses of plant extracts to inhibit cultured skin cell division, since skin thickening is one of the primary symptoms of psoriasis. We found that herbs that are regarded as highly important in Arabic dermatological medicine performed very well in these assays, showing a major difference between cytostatic and cytotoxic effects. Black cumin or black seed (Nigella sativa, Ranunculaceae) was one such plant. Using the results from this research, as well as published data and extensive exploration of Arabian medicine texts and current traditional practice, a synergistic combination of specific plant parts of several herbs was developed. Nigella not only acts against skin thickening, but it also has significant and well-documented anti-inflammatory and antiseptic effects.30,31 Other herbs are added for anti-itching, pain-relieving, and anti-inflammatory effects, and to support the tissues and skin condition.
(b)Acne: Acne vulgaris results from excess production of sebum in the sebaceous glands due to hormonal, environmental, or other factors. Anaerobic bacteria feed on the sebum creating a local infection and associated inflammatory response, which is seen as unsightly spots. We used a sophisticated screening method of measuring sebum production in sebaceous glands isolated from human skin and maintained in organ culture in the laboratory. According to some unpublished observations by Y. Nissimov and Y. Milner at the Meyer’s Skin Biochemistry Research Laboratory, Hebrew University in Jerusalem, several herbs based on Arabic medicine treatments for spots were able to suppress sebum production, in some cases almost completely. In addition, we collaborated with Professor Ali-Shteya in the Microbiology Department at An-Najah University in Nablus, Palestine to identify herbs with powerful antibacterial action on the anaerobic bacteria involved in acne, Propionibacterium acnes. We found at least 2 herbs, soapwort (Saponaria officinalis, Caryophyllaceae) and Inula viscosa (Asteraceae), which had powerful antimicrobial effects against this bacteria. Combinations were made from these herbs, in which one herb stopped sebum production and cleaned the skin, another prevented growth of anaerobic bacteria, and a third provided mild antiinflammatory skin conditioning and astringent effects to support skin quality.
The above are synergistic combinations, rationally formulated according to both traditional Arabic medicine and modern scientific research. They may have an advantage over the use of single herbs such as calendula (Calendula officinalis, Asteraceae), tea tree (Melaleuca alternifolia, Myrtaceae) oil, lavender (Lavandula angustifolia, Lamiaceae) oil, chamomile (Matricaria recutita, Asteraceae), witch hazel (Hamamelis virginiana, Hamamelidaceae) and Aloe vera (Liliaceae), which may have a onedimensional activity, such as anti-inflammatory, astringent, antiseptic, or antioxidant effect.
Conclusion
Many of the herbal combinations for various common health problems have now been tested in clinical studies among the Arab population of the Galilee, and there are a series of scientific publications already out or on the way. In addition, a major international company based in Denmark (Sprunk-Jansen Ltd.)32 has taken these product concepts and is marketing them internationally. They are already in 20 countries so far. The project is not just about marketing a radically new line of effective herbal combinations but the introduction of Arabic medicine itself as a whole new modality into Western markets. This may have unexpected advantages. For example, according to current European regulations, herbs which have not previously been consumed in Europe cannot be sold as they are regarded as ‘novel foods.’ However, many herbs offered through Arabic medicine, such as black cumin/ black seed, are already known, consumed by communities in the EU area, and though entirely novel as medicines, are permitted. Arabic medicine can therefore help to return innovation into the European herbal market.
How does all this help peace and co-existence? All projects in which Jewish and Arab professionals cooperate create important precedents and a sense of normalization. But herbal remedies do more than that. They carry an emotional message of cultural empowerment and community selfcare. When one of us gave talks on Arabic herbs in the Palestinian town of Nablus, the older women from the surrounding villages began to weep. They explained that under the Israeli occupation and with the pressures of modern life, their traditional cultural knowledge was disappearing. Violence and despair increased without this support. Teachings on herbs and family healthcare skills restored a sense of ownership and legitimacy to their culture and their community. Stephen Fulder, PhD, has worked for 30 years as a consultant to companies in the herbal field and has lectured at universities and many international conferences. He has written 14 books and approximately 40 academic papers regarding herbs and natural medicine. He lives in Galilee, Israel in an environmental village that he helped to found, and he is active in peace and environmental work. He earned his doctorate in the molecular biology of aging from Oxford University. Omar Said, PhD, is the founder and CEO of Antaki Center for Herbal Medicine Ltd, a company established in 1998 that develops a wide variety of medicinal herbal formulations based on traditional Arab medicine. He serves as the head of the medicinal plant project in the Galilee Society R&D regional center, as well as the manager of Al-Maissam—The Medicinal Plant Center for Research & Education. He obtained his doctorate in pharmacology from the Technion, Institute, Haifa, Israel.
Conflict of Interest Disclosure Dr. Fulder is an independent consultant, author, and researcher, with no interest in or ownership of the project and organizations mentioned and will have no benefit from any interest generated by this article. Dr. Said is a part owner of the Antaki Company, which is mentioned and could possibly benefit from interest generated by the article, but very indirectly, as Antaki Ltd. does not market finished products outside Israel. *Cana of Galilee, famous as the Christian pilgrimage site of Jesus’s miracle of changing water into wine. †In the Arabic translations of Dioscorides, of which there are many throughout the ages, impotence is described and recommended remedies included plants in the genus Ferula. This plant’s description as well as its specific Arabic name clearly identifies it as Ferula, but there is uncertainty concerning the exact species. One can never be sure of the precise botanical identification of an ancient common name. However, in the ethnopharmacological research in the Middle East that these authors have conducted, F. communis is known and used, but not once mentioned for treatment of impotence, whereas F. hermonis is widely known and used for impotence. Therefore it is reasonable to suggest it is this species.
References
- Medicinal Plant Center page. The Galilee Society Web site. Available at: http://www.gal-soc.org/en/?s=Al-Maissam. Accessed May 4, 2009.
- Saad B, Azaizeh H, Said O. Tradition and perspectives of Arab herbal medicine: A review. eCam. 2005;2:475–479.
- Levey N, Khaledy N. The Medical Formulary of al-Samarqandi. University of Pennsylvania Press; 1976.
- Said O, Khalil K, Fulder S, Azaizeh H. Ethnopharmacological survey of the medicinal herbs in Israel, the Golan Heights and the West Bank Region. Journal of Ethnopharmacology. 2002;83:251–263.
- Ali-Shtayeh MS, Yaniv Z, Mahajna J. Ethnobotanical survey in the Palestinian area: a classification of the healing potential of medicinal plants. Journal of Ethnopharmacology. 2000;73:221–232.
- Lev E. Reconstructed materia medica of the Medieval and Ottoman al-Sham. Journal of Ethnopharmacology. 2002;80:167–179.
- Lev E, Amar Z. Ethnopharmacological survey of traditional drugs sold in Israel at the end of the 20th century. Journal of Ethnopharmacology. 2000;72:191–205.
- Heneidy SZ, Bidak LM. Potential uses of plant species of the coastal Mediterranean region, Egypt. Pakistan Journal of Biological Sciences. 2004;7:1010–1023.
- Arab Union for Agriculture and Development: The Neglect of Medicinal Plant Resources in the Arab World. A Report. Cairo, Egypt. 2000.
- Abu-Irmaileh BE, Afifi FU. Herbal medicine in Jordan with special emphasis on commonly used herbs. Journal of Ethnopharmacology. 2003;89:193–197.
- Said O. (unpublished data, 2008)
- Department of Ecology at the Hebrew university of Jerusalem. Checklist and ecological data-base of the flora of Israel and surroundings, Rotem. 1999.
- Palevitch D, Yaniv Z. Medicinal Plants of the Holy Land. Tel Aviv, Israel: Modan Publishing House; 2000.
- Shmida A, Fragman A. Endangered and rare plant species of Israel. Ecology and Environment, Israel (Hebrew); December 1999.
- Antaki Center for Herbal Medicine Ltd Web site. Available at: www. al-antaki.com.
- Ibn Wahshiya, The Book of Nabatean Agriculture. (3 volumes). (Edited by Prof. Tawfiq Fahd), Aljaffan and Al Jabi publisher, Limassol, Cyprus, and Damascus, Syria,1993. (In Arabic)
- Bailey C, Danin A. Beduin plant utilization in Sinai and the Negev. Economic Botany. 1981;35:145–162.
- Dafni A, Yaniv Z, Palewitch D. Ethnobotanical survey of medicinal plants in northern Israel. Journal of Ethnopharmacology. 1984;10:295–310.
- Yaniv Z, Dafni A, Friedman J, Palewitch D. Plants used for the treatment of diabetes in Israel. Journal of Ethnopharmacology. 1987;19,145–151.
- Friedman J, Yaniv Z, Dafni A, Palewitch D. A preliminary classification of the healing potential of medicinal plants based on a rational analysis of an ethnopharmacological field survey among Bedouins in the Negev desert, Israel. Journal of Ethnopharmacology. 1986;16:275–287.
- Kalderon B, Gutman A, Levy F. et al. Characterisation of stages in development of obesity-diabetes syndrome in sand rat (Psammomys obesus). Diabetes. 1986;35: 717–724.
- Shani J, Ahronson Z, Sulman FG. et al. Insulin-potentiating effect of the salt bush (Atriplex halimus) ashes. Israel Journal of Medical Sciences. 1972;8:757–8.
- Mertz W, Roginski EE, Gordon WA, et al. In vitro potentiation of insulin by ash from saltbush (Atriplex halimus) Arch. Int. Pharmacodyn. Ther. 1973;206:121–128.
- Said O, Fulder S, Khalil K et al. Maintaining a physiological blood glucose level with ‘Glucolevel’, a combination of four antidiabetic plants used in Traditional Arabic Herbal Medicine. eCam. 2008;5:421–8.
- Ibn Albitar. In: Aljamea Limufradat Aladwiya Walaghdiya, p. 115–116. Dar Bulaaq, Cairo 1974. (Manuscript from 12th Century).
- Zanoli P, Benelli A, Rivasi M, et al. Opposite effect of acute and subchronic treatments with Ferula hermonis on copulatory behavior of male rats. Int J Impot Res. 2003; 15(6):450–5.
- Homady MH, Khleifat KM, Tarawneh KA, et al. Reproductive toxicity and infertility effect of Ferula hermonis extracts in mice. Theriogenology. 2002;57(9):2247–56.
- Khleifat KM, Homady MH, Tarawneh KA, et al. Effect of Ferula hermonis extract on social aggression, fertility, and some physiological parameters in prepubertal male mice. Endocr J. 2001;48(4):473–82.
- Kassis E, Fulder S, Khalil K, et al. ‘Masculine’ is a proprietary extract of Ferula asafetida to enhance male sexual functioning in animals and man. (submitted).
- Khan M. Chemical composition and medicinal properties of Nigella sativa Linn. Inflammopharmacol. 1999; 7: 15–35.
- Al-Ghamdi MS. The anti-inflammatory, analgesic and antipyretic activity of Nigella sativa. J Ethnopharmacol. 2001; 76: 45–48.
- Sprunk-Jansen Web site. Available at: www.sprunk-jansen.com. Accessed May 4, 2009.
|
|
|
|
|
|
|